
Retrosternal, substernal and intrathoracic goitre is a subgroup of multinodular goitre (MNG). The most commonly recognised and appropriate term is intrathoracic goitre (IG) and for the purpose of this chapter this is the term that is used.
IG presents specific challenges in relation to preoperative evaluation and surgical management. Classic indications for sur-gery include pressure and cosmetic effects, and higher-than-expected rates of incidental malignancy in a MNG with retrosternal and intrathoracic extension.1

MNG refers to an enlarged thyroid gland with multiple nodules. Challenges specific to MNG include evaluating the patient, determining the risk of malignancy within the multiple nodules, selecting patients who require surgery, and planning an appropriate surgical approach to address the disease without undue risk of complications. MNG is generally presumed to be a response to oversecretion of Thyroid Stimulating Hormone (TSH).
The thyroid hyperplasia is probably due to reduced production of thyroid hormones relative to the metabolic demand of the body. This can be due to a congenital or an acquired defect. Morphological and molecular studies suggest a degree of polyclonal aetiology. MNGs are sometimes familial and one study suggests linkage to a DNA mother as chromosome 14q 2.
Not all MNGs require surgery. Palpable nodules occur in 4-7% of adults 3. With the advent of high resolution ultrasound (USS), nodules and nodular thyroids are detected in 50-70% of adults 4. In non-iodine deficient patients, ultrasound can detect thyroid nodules in >20% of people, and multiple nodules in 9%. Rates are higher in females and in older patients 2, 4. This suggests that an increasing number of patients with MNG will be encountered in an ageing population.
Haller first provided an anatomical description of the IG in 1794; since then it has been given a number of names and descriptions e.g. retrosternal, substernal, retroclavicular and intrathoracic goitre. Numerous classifications have been used (Table 1). Authors have compared these definitions in an attempt to define its utility and allow for sensible comparisons 5. Huins et al indicated a need to apply 3 grades depending on the relationship of the IG to the aortic arch and the right auricle.
More recently Rios et al critically analysed all classifications to determine the most useful definition of IG for predicting intra-operative as well as postoperative complications. They found that most definitions can be ignored as they are not clinically relevant and concluded that Katlic’s definition 6 was the most useful for predicting the need for a possible sternotomy to remove an IG 7.

For a thyroid gland to reach sufficient size to pass into the mediastinum, the pathological processes involved must have been present for many years. It is therefore unsurprising that the vast majority of surgical specimens demonstrate benign pathology. The rate of malignancy in reported surgical series is low (6-21%) 8, 9, 10, 11. However, it is important to consider malignancy as it may significantly alter management.
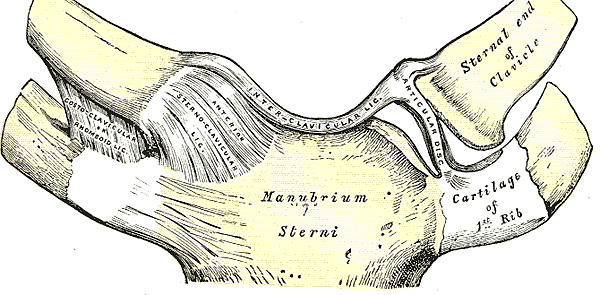
It is not uncommon for IG to manifest in the elderly and many patients are relatively asymptomatic. The thoracic inlet, bound by the clavicles, 1st rib, sternum and vertebrae contains many vital structures. In addition to the prevertebral muscles, the trachea, oesophagus, carotid and jugular vessels all pass through this region. As the thyroid gland enlarges, an increasing percentage of the cross-sectional area of the inlet is occupied by the goitre, leaving less room for other structures. Pressure symptoms tend to develop in low-pressure areas in the first instance, and a feeling of difficulty swallowing is a common initial symptom. As the compression increases, along with increasing dysphagia, pressure on the trachea can lead to deformity of the tracheal rings and airway compression. In extreme cases, pressure on the venous structures of the neck can cause superior vena cava syndrome, although this is rare (5%) 8. It manifests with distension of the veins in the neck, oedema of the face and arms, shortness of breath and dysphagia. Elderly patients often have unrelated comorbidities and require a thorough preoperative evaluation and careful surgical planning and technique.
Airway management may not be straight-forward, although truly difficult intubations are uncommon 9. Cooperation between surgeon and anaesthetist is crucial to avoiding problems at this critical stage of the procedure. The majority are amenable to endotracheal intubation, as the endo-tracheal tube stents the trachea open.
Some patients have symptoms that vary with head position. With the neck fully extended, the goitre is pulled upwards towards the thoracic inlet, and this might compromise the airway. In such cases an awake fibreoptic intubation may be required to allow the neck to be flexed during intubation.
Tracheomalacia is caused by longstanding pressure on the trachea, and becomes evident only on completion of surgery. It manifests as stridor following extubation. It is uncommon, and postoperative tracheastomy is rarely required (2%); tracheostomy is more commonly required following traumatic intubation causing oedema rather than for tracheomalacia 9.
Appropriate management should take into consideration the size of the goitre, the degree of aerodigestive tract compression, concerns about malignancy, and comorbidities.
With compressive symptoms, surgery provides the only means of relief and provides tissue for histological analysis. For the few patients with malignancy, resection is the mainstay of therapy, and permits adjuvant radioiodine treatment to be used when indicated.
Indications for surgery in patients in whom IG is incidentally found are unclear. As imaging becomes more widely used, an increasing number (up to 40%) of IGs are detected incidentally during work-up of other diseases 8, 10. Some authors consider the mere presence of an IG as an indication for surgery 9 whereas others question the need for surgery in all cases especially if malignancy is not suspected 11. Decision-making regarding surgery in such patients should be individualised. For example, a patient with an asymptomatic IG detected on imaging to stage an incurable aggressive malignancy clearly is not a candidate for surgery. In contrast, an otherwise well patient with asymptomatic tracheal compression and an excellent life expectancy will be a good surgical candidate. Surgery in this clinical setting prevents progression of airway symptoms.
The difficult patient is one with little/no comorbidities and asymptomatic disease, with early tracheal compression. Such patients should be made aware of the risks and benefits of both a conservative and a surgical approach. Interval imaging often provides critical information about the trajectory of the disease which assists with decision making in borderline cases.
Once it has been decided that surgery is indicated, then preoperative evaluation focuses on the following:
Comorbidities: Because many patients are elderly, those requiring an extracervical approach (sternotomy or thoracotomy) need to be carefully assessed as to their general fitness for surgery. Electrocardio-graphy, echocardiography and assessment of lung function should be considered in those requiring sternotomy, and in all other patients with significant cardiorespiratory disease as part of assessment prior to anaesthesia.
Assessment of thyroid tumour: Patients should have a full head and neck examination with particular focus on the presence of cervical lymphadenopathy. Ultrasound is used to assess the central and lateral neck.
Fine Needle Aspiration Cytology (FNAC): Even though the incidence of malignancy with retrosternal MNG is low, (ultrasound-guided) FNAC assessment may identify malignancy preoperatively and allow for better counselling and pre-operative planning of the extent of surgery.
Thyroid and parathyroid function: Thyroid function tests and serum calcium levels are done. Hyperthyroid patients with are medically managed to achieve euthyroidism prior to surgery to prevent a life threatening thyrotoxic crisis during or after surgery. This usually involves thionamide antithyroid drugs, or potassium iodide (40mg three times daily for 10 days) +/- beta-blockade (e.g. propranolol 40 - 80mg three times per day).
Vocal cord function: Assessing vocal cord function by indirect or flexible laryngos-copy in the awake patient is essential, not only for medicolegal reasons, but also to determine the function of the contralateral RLN to pre-empt possible airway compromise postoperatively.
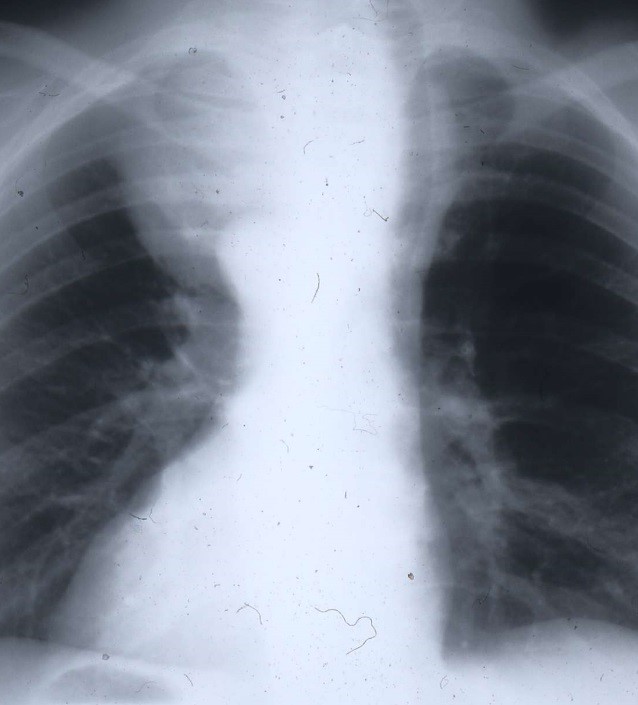
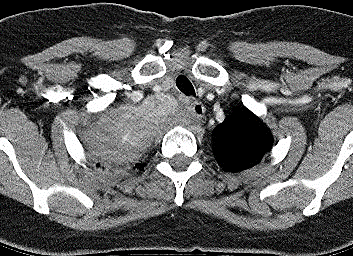
Imaging the trachea: In patients with stridor due to tracheal compression, imaging is required to determine the site and length of the tracheal narrowing both for the anaesthetist and the surgeon. Even though CT or MRI is preferred, an AP X-ray may give a good indication (Figure 3).
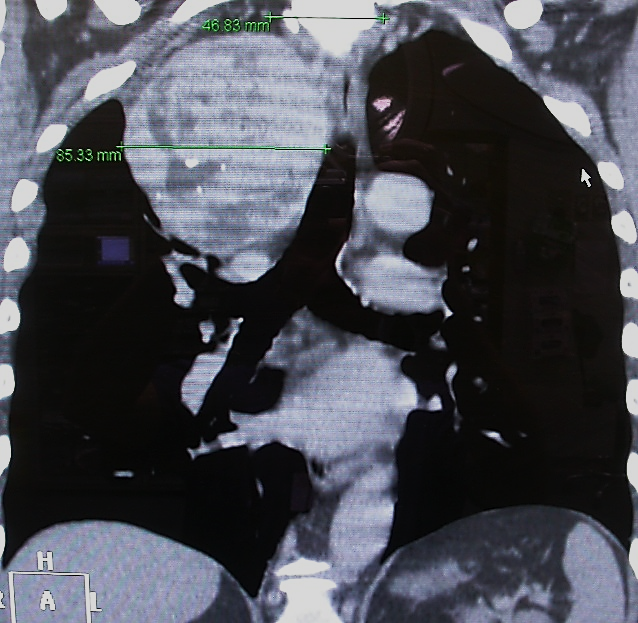
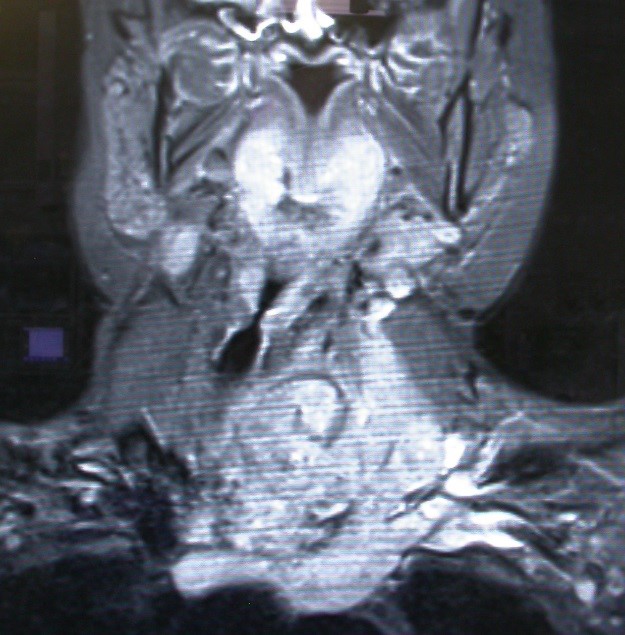
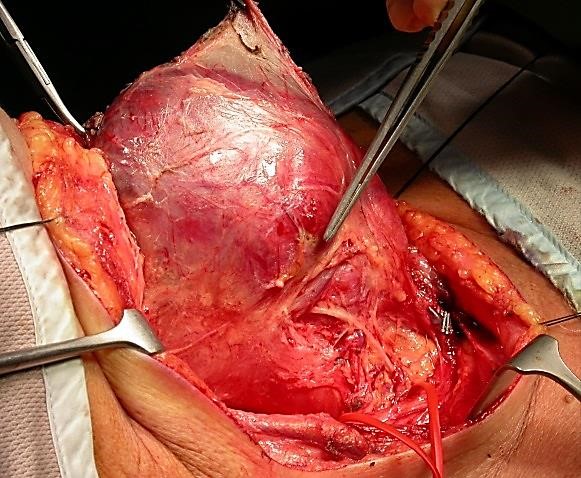
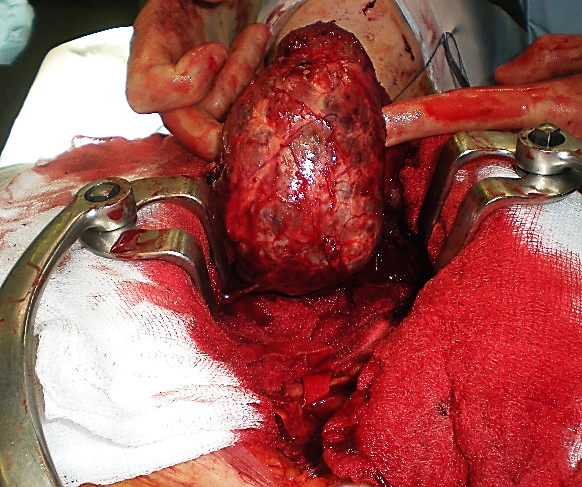
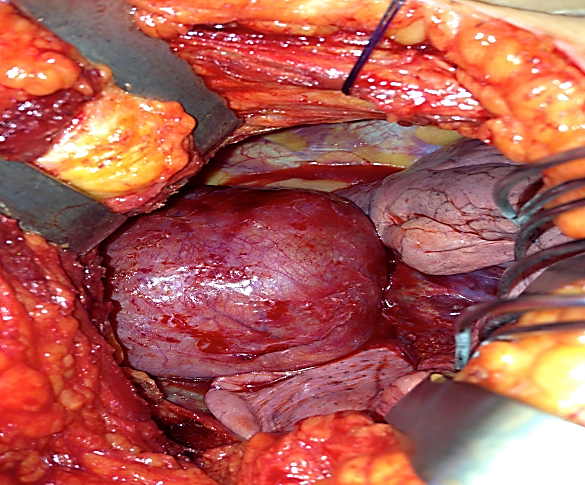
Imaging the mediastinum (Figures 4, 5): The relationship of a goitre to the trachea, oesophagus and great vessels is readily appreciated on imaging, and guides the surgical approach (cervical +/- sternotomy) which may require the input of other surgical teams, as well as provides invaluable information to the anaesthetist about the presence of laryngotracheal compression and likely problems with endotracheal intubation.
Patients with (suspected) retrosternal thy-roid should have cross-sectional imaging (CT or MRI) with intravenous contrast to define its size, position and anatomical relationships to mediastinal structures. Imaging helps to demonstrate the tissue planes surrounding the thyroid mass. Any evidence of extrathyroidal extension should be considered as evidence of malignancy and the surgical approach tailored accordingly 8.
Coagulation status: Exclude clotting dis-orders to reduce bleeding, discontinue anti-coagulants e.g. warfarin or clopidogrel and substitute with heparin if required.
Multidisciplinary team meeting: Once a patient satisfies the indications for IG surgery the multidisciplinary team must set aside time to ensure that the patient and conditions are favourable to proceed and to plan to minimise complications. IG can be associated with significant laryngotracheal compression resulting in difficult orotracheal intubation. Prior to surgery, the surgeon and anaesthetist must discuss the air-way plan and jointly review the imaging.
Informed consent is essential. Complication rates from IG surgery are low in experienced hands, but when they do occur they may be associated with significant morbidity and/or mortality. Patients need to be aware of these risks, especially in the context of an asymptomatic patient with benign disease who may elect to delay surgery and be managed conservatively. However in the context of retrosternal goitre, patients should also be aware that with continued growth, delaying an operation may make future surgery technically more challenging, thus potentially increasing the risk of complications.
Prior to discussing specific risks of surgery, patients are informed of general anaesthetic (GA) risks. When the goitre is associated with significant tracheal compression, orotracheal tube intubation may be difficult, and patients should be enlightened that initial airway management may be challenging, though with appropriate preoperative planning and medical/surgical personnel, this should not be insurmountable.
IG surgery is associated with a number of potential life-threatening complications although in specialised centres complication rates are usually low (<5% for bleeding, infection, permanent recurrent laryngeal nerve (RLN) and external branch of superior laryngeal nerve (EBSLN) paralysis and hypoparathyroidism) 12, 13. However it is important that the operating thyroid surgeon regularly audits his/her own complication rates, and informs patients of their own outcomes.
The functional implications of RLN palsy include altered voice, aspiration, or airway obstruction if bilateral. EBSLN palsy may also cause vocal fatigue and impairment of voice pitch and projection. Unrecognised hypoparathyroidism and consequent hypo-calcaemia may be life threatening. Permanent hypoparathyroidism requires lifelong calcium +/- vitamin D supplementation. In addition, patients need to be made aware of the need for lifelong thyroxine with total thyroidectomy, and unless undergoing a robotic or other minimally invasive approach, that they will have a neck scar that in some ethnic groups, such as Asians or Afro-Caribbeans may become hypertrophic or form keloid. Regardless of surgical approach, there will also be numbness above or below the incision and that may be permanent.
IT surgery may require median sternotomy to remove the superior mediastinal component. Thoracic surgeons usually perform the sternotomy. Patients need to be aware that although uncommon (<5% of patients) complications from median sternotomy may include trauma to mediastinal structures, pneumothorax, pneumomediastinum, mediastinitis, sternal dehiscence, and osteomyelitis.
Patient position: We previously alluded to possibly worsening airway obstruction by extending the neck; this situation may require blind fibreoptic intubation in an awake patient.
Intubation technique: Extrinsic tracheal compression is generally ‘soft ‘in nature and can easily be overcome by gentle insertion of an endotracheal tube, which may need to be one size smaller than what is usually used for a patient. Occasionally a stiff introducer may be required to forcefully advance the tube past a narrowed tracheal segment. To avoid the dreaded emergency scenario of ‘can’t intubate, can’t ventilate’ at induction of anaesthesia in a paralysed patient, the anaesthetist may choose to perform an awake fibreoptic oral/nasal tracheal intubation with the aid of topical local anaesthesia.
Choice of endotracheal tube: The anaes-thetist must be aware of the presence, degree and level of compression of the trachea to select and appropriate diameter, and length of tube. A double lumen endo-tracheal tube may be required to permit selective pulmonary ventilation. Cases where extensive mediastinal dissection is anticipated require an experienced anaesthetist with appropriate head and neck or thoracic anaesthetic expertise, as these tubes can be challenging to place in patients with a difficult airway.
Neuromonitoring: Neuromonitoring of the recurrent laryngeal nerve reduces palsy rates with difficult thyroidectomy, such as in retrosternal goitre surgery. 14 Where nerve monitoring is to be employed, long-acting muscle relaxants must be avoided so as not to interfere with neural monitoring; short acting agents can be used for induction of anaesthesia.
Extubation: At the end of surgery, tracheal compression from a longstanding goitre may cause a degree of trachea-malacia; in our experience extubation is almost always possible. In the highly unlikely event that the patient experiences airway obstruction on extubation due to tracheomalacia, the patient should be reintubated for a minimum of 72h until a leak is observed around the endotracheal tube and a tracheostomy performed if necessary. 20
Postoperative monitoring: Patients with significant cardiorespiratory disease requiring median sternotomy are at higher risk of postoperative complications and require close monitoring after surgery in a high dependency or intensive care setting.
Surgery for IG poses significant intra- and postoperative challenges and should ideally be done by experienced surgeons who are part of a multidisciplinary team, and have the knowledge and ability to deal with intra- and postoperative complications of the surgery.
Total vs hemithyroidectomy?
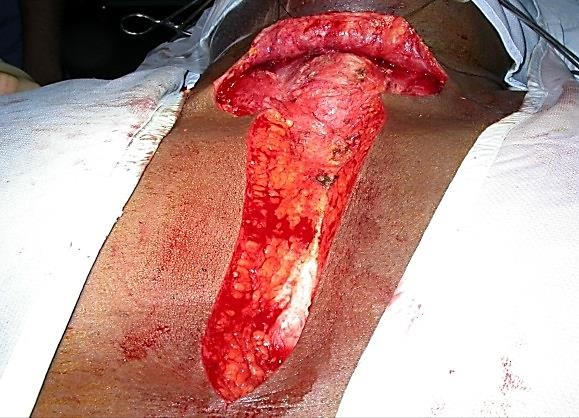
Total thyroidectomy is indicated for bilateral thyroid gland enlargement. However in patients with unilateral enlargement or in whom there is a significant risk to the RLN or parathyroid function, thyroid lobectomy is a perfectively acceptable option as the majority of goitres will be benign. 9
Total thyroidectomy is also contraindicated in settings where thyroid and/or calcium replacement therapy and monitoring is not possible as is the case in many developing countries.
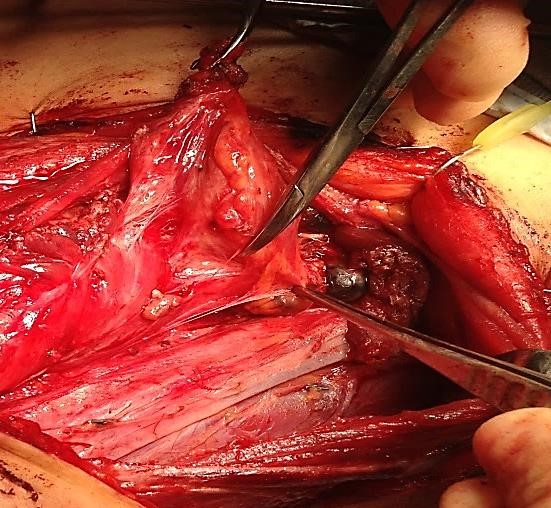
Management of RLN: The RLN should always be identified. With large goitres, localisation of the nerve can be challenging due to distortion of the anatomy. It is not uncommon for the nerve to be riding over a hyperplastic nodule, making it particularly vulnerable. With this in mind surgeons must be familiar with localising the RLN either at the cricothyroid joint (Figure 6) or laterally at the level of the inferior thyroid artery (ITA).
Neuromonitoring: Neuromonitoring for neoplastic MNG is a valuable technique to identify and safely preserve the RLN.
Parathyroid glands: It is imperative to ensure that every effort is made to identify and preserve at least the superior glands which have a more constant anatomical position in close relationship with the ITA. With surgery for large MNGs the para-thyroids may be displaced due to aberrant growth of the thyroid gland.
Berry’s ligament: Dissection of Berry’s ligament is one of the most delicate steps of thyroid surgery due to its vascularity and close relationship to the RLN. It is imperative that minimal traction be applied when holding the thyroid lobe to avoid traction injury to the nerve. The ligament is dissected from the nerve with fine instruments, usually with judicious use of bipolar diathermy and fine scalpel dissection.
The following surgical approaches will now be described:
Surgery for MNG can be challenging due to distortion of anatomy, difficult exposure, and involvement of vital structures.
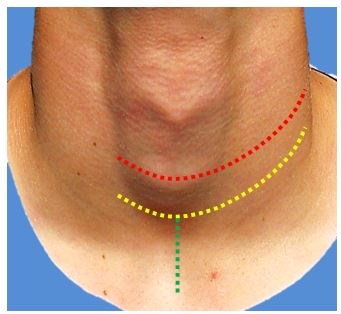
If however, a lateral neck dissection is done then a modified extended Kocher incision is preferred (Figure 7); this a similar incision as described above, other than that the incision is placed centered over the cricoid prominence to permit exposure of the neck up to the mandible. If a midline sternotomy is required then a minor vertical incision is added (Figure 7)
Extracervical approaches require an understanding and experience of surgical techniques to access the mediastinum and the pleural spaces as well as having a dedicated and expert multidisciplinary team including (cardio)thoracic surgeons.
Combined Cervical & Midline Sterno-tomy
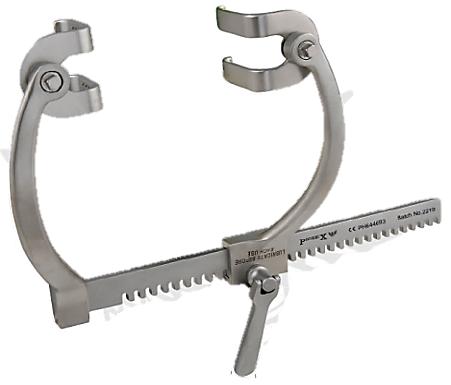
Indications for sternotomy are based on the anatomical relationship of the goitre to me-diastinal structures. The indications have already been described above. It comprises 3 main stages:
This approach has 2 main stages:
It is indicated when a goitre extends into the posterior mediastinum and reaches the posterior pleura and a midline sternotomy would not provide enough space to dissect the goitre from such a posterior location (Figure 13).
Postoperative complications are infrequent in experienced units, but need to be recognised and managed timeously to minimise morbidity and mortality.
With bilateral surgery, transient or permanent bilateral RLNs paralysis may cause life threatening airway obstruction. It may not always be immediately evident following extubation, but should be suspected with stridor and respiratory compromise following total thyroidectomy, or with a unilateral procedure in a setting of pre-existing contralateral RLN palsy. In cooperative patients, flexible laryngoscopy confirms the diagnosis. Management depends on the degree of respiratory compromise and the surgeon’s level of confidence that the RLN paralysis is transient or permanent. This is why neuromonitoring is useful, as a nerve for which an intact monitoring circuit had been confirmed with pre- and post-dissection vagal stimulation will invariably recover 15. A decision then has to be made to either to institute conservative measures (e.g. supplemental oxygen, adrenaline nebulisers) and to closely monitor the patient’s airway, or to reintubate the patient or to do a tracheostomy.
Bleeding may manifest as increased drain output (e.g. >100mls in <1 hour) and/or an expanding neck haematoma. Both situations require immediate re-exploration of the neck to arrest bleeding to avoid both airway and cardiovascular compromise. Most haematomas occur in the 1st 24 hours; bilateral surgery has a higher risk compared to thyroid lobectomy. Life-threatening haematomas are uncommon and occurs in <1% of cases. 31 Preoperative evaluation should have identified patients at high risk of bleeding such as those on anticoagulants. An expanding neck haematoma reduces venous return, and can quickly cause airway obstruction due to laryngeal oedema. Management includes early recognition and immediate evacuation of the haematoma and arresting the source of the bleeding. Airway management may require a tracheostomy or cricothyroidotomy if endotracheal intubation is unsuccessful.
The parathyroid glands may inadvertently be removed even by experienced surgeons. The excised thyroid gland should carefully be inspected for the presence of parathyroid glands that should then be re-implanted into the sternomastoid muscle. Hypoparathyroidism needs to be detected to prevent cardiovascular and neurological complications from hypocalcaemia. Following total thyroidectomy, it is common practice to check the adjusted serum calcium levels 6 and 12 hours postoperatively. Levels <1.9mmol/L should prompt intravenous calcium to be administered (usually 10mls of 10% calcium gluconate over 10-15 minutes) to prevent cardio-vascular and neurological consequences of hypocalcaemia. When the surgeon strongly suspects that the parathyroids were compromised during surgery e.g. following central compartment neck dissection, one may elect to commence oral calcium supplements +/- vitamin D immediately post-operatively. Serum parathyroid hormone (PTH) levels can be checked to determine the need for long-term oral calcium supplementation. Patients sent home on oral calcium should be closely followed up to ensure that an appropriate early calcium weaning protocol is followed in patients (majority) that recover normal parathyroid function.
Seromas may be reduced if neck drains are used 16, and not removed too early. Despite appropriate drain management, seromas however still occur. Seromas usually settle within 4-6 weeks. Active management by repeated aspiration is only required when for compressive symptoms or cosmetic concerns.
Because thyroidectomy is a “clean” operation, infection is uncommon and prophylactic antibiotics are not recommended 13. When it does occur, it usually settles with antibiotics that cover Staphylococcal and/ or Streptococcal bacteria. Very rarely is incision and drainage of an abscess required.
Voice change occurs commonly following thyroidectomy. It is not necessarily due to injury to the RLN, but is often caused by laryngeal oedema from the endotracheal tube, and postsurgical venous congestion of the larynx. Apart from altered voice that occurs with RLN injury, patients may experience swallowing difficulty, aspiration, and life-threatening stridor with bilateral RLN paralysis
Vocal cord paralysis due to RLN injury is a potentially serious complication. In cases of retrosternal goitre, the external branch of the superior laryngeal nerve (EBSLN) and RLN are at greater risk due to being displaced by the tumour; this makes anatomical recognition more difficult. Additionally the manoeuvres required to deliver a large goitre render the RLN more susceptible to stretching or compression.
Always examine the vocal cords at follow-up not only to assess functional outcome of the surgery, but also because of implications of a paralysed RLN for swallowing and future contralateral surgery.
When the RLN has obviously been transected intraoperatively, most agree that a tension-free repair of the RLN should be performed.
Airway and swallowing dysfunctions are managed in the perioperative period depending on the status of the contra-lateral RLN. However, when vocal cord paralysis occurs when the RLN was noted to be anatomically intact at completion of surgery (+/- normal function confirmed with neuromonitoring), then re-exploration is not indicated as the paralysis is invariably temporary. Dexamethasone may possibly reduce the rate of temporary RLN palsy 17.
With bilateral RLN injury, airway compromise is to be expected. Management is dictated by the intraoperative assessment of the RLNs. If the nerves were intact, then patients should be reintubated and managed in a critical care setting with intravenous steroids and a trial of extubation attempted after 48 hours.
Voice therapy by a speech and language therapist/pathologist is an essential aspect of management of RLN or EBSLN injury. Principles of voice therapy include ensuring understanding and knowledge of laryngeal function and rationale of therapy; voice care, managing glottal insufficiency; improving vocal fold adduction; reducing transglottic airflow and improving subglottic air pressure; preventing supraglottic hyperfunction; optimising resonance and pitch; reducing aspiration; and improving airway clearance. This is best initiated as early as possible for best outcomes. In a small minority of patients with permanent unilateral vocal cord paralysis that do not respond to voice therapy, a variety of vocal cord medialisation procedures can improve voice and swallowing.
Most patients in whom bilateral RLN injury is recognised intraoperatively require immediate tracheostomy to secure a safe airway. Further management depends on patient and tumour factors. Further interventions may not be indicated in patients with advanced disease or significant comorbidities. Laser cordotomy may allow decanulation of fit, motivated patients with reasonable pulmonary reserve.
Hemithyroidectomy is associated with a 12 - 35% risk of hypothyroidism. 18, 19 Hence patients should have thyroid functions checked within 6 - 8 weeks. Risk factors for hypothyroidism include high-normal serum TSH levels, lower free thyroxine levels and Hashimoto’s thyroiditis. 20, 21 Lifelong thyroid hormone replacement is required following total thyroidectomy, usually in the form of oral levothyroxine, with doses adjusted over a 2 - 8 weeks to achieve optimum therapeutic levels.
Tracheomalacia refers to weakness of the tracheal wall following resection of a goitre. Although weakness of the cartilaginous trachea has been attributed to long-standing compression causing ischaemic damage, the pathophysiology remains poorly understood.
Tracheomalacia causing airway obstruction is very rare. A soft, easily collapsible trachea following goitre resection should be noted on palpation, following which a tracheostomy should be performed to secure the airway. If tracheomalacia was suspected intraoperatively and the patient develops airway obstruction following extubation, it is important to exclude bilateral RLN paralysis. If bilateral RLN paralysis has been excluded, repeat endo-tracheal intubation is done with a trial of extubation after 48hrs. Waiting 48hrs allows paratracheal fibrosis to occur that reduces tracheal collapse from negative intratracheal pressures. However one should have a low threshold for tracheostomy for medium to long-term airway management.
Thyroidectomy
https://vula.uct.ac.za/access/content/group/ba5fb1bd-be95-48e5-81be-586fbaeba29d/Thyroidectomy.pdf
Parathyroidectomy
https://vula.uct.ac.za/access/content/group/ba5fb1bd-be95-48e5-81be-586fbaeba29d/Parathyroidectomy.pdf
Ricard Simo FRCS (ORL-HNS)
Consultant Otorhinolaryngologist, Head & Neck Surgeon
Guy’s and St Thomas’ Hospital NHS Foundation Trust and Honorary Senior Lecturer Guy’s King’s and St Thomas’ Medical School
London, United Kingdom
ricard.simo@gstt.nhs.uk
Iain J. Nixon, MBChB, FRCS (ORL-HNS), PhD
Consultant Otorhinolaryngologist, Head & Neck Surgeon
Edinburgh Royal Infirmary
United Kingdom
iainjnixon@gmail.com
Enyunnaya Ofo FRCS (ORL-HNS), PhD
Consultant Otorhinolaryngologist, Head & Neck Surgeon
St George’s University Hospital
London, United Kingdom
eofo@hotmail.com
Johan Fagan MBChB, FCORL, MMed
Professor and Chairman
Division of Otolaryngology
University of Cape Town
Cape Town
johannes.fagan@uct.ac.za