Pathology in the nasopharynx can be addressed endoscopically, or as an open procedure. The advantage of an open procedure is that it affords better surgical access. There are a variety of open approaches to the nasopharynx inter alia transnasal, transmaxlary, infratemporal fossa and transpaltal approaches.
The maxillary swing approach is a variation of the transmaxillary approach and provides wide access to the nasopharynx as well as to the pterygopalatine fossa and pteygomaxillary fissure; it also preserves soft palate function which is so vital for speaking and swallowing.
Preoperative consent includes but is not limited to facial incisions, loss of sensation in the infraorbital nerve distribution, loss of maxillary bone, wound dehiscence and breakdown, oronasal and oronasopharygeal fistulae and ectropion.
A tracheostomy is routinely performed either under local anaesthesia or following administration of a general anaesthetic. Perioperative antibiotics are given on induction of anaesthesia.
The patient is positioned supine and the head supported with a head ring. The eyes are protected according to the institution’s protocol. An ocular lubricant or ointment is inserted into both eyes such as chlormyctin eye ointment if the patient is not allergic to it. The contralateral eye may be covered with a transparent protective adhesive dressing and a tarsorrhaphy performed on the ipsilateral eye taking care not to invert the eyelashes so as to avoid corneal abrasions.
The patient’s face and neck are prepped; an alcohol based solution or other solutions that may irritate the eyes or to which the patient is allergic should not be used. The oral cavity is prepped. The nasal cavity is packed with topical vasoconstrictor-soaked ribbon gauze.
The scalp, lower neck and chest are draped leaving the forehead, face, upper neck and both ears exposed.
The operation may be considered in 3 stages:
It is important to complete the soft tissue dissection and bone exposure before doing any bone work so as to avoid excessive blood loss.
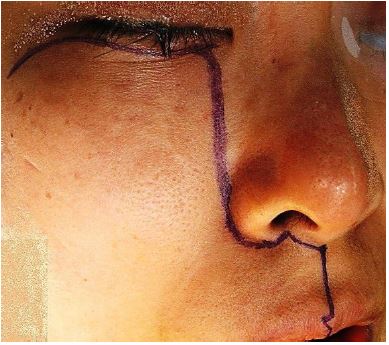
Using a sterile marking pen, draw an incision line 5mm below and parallel to the lower eyelid lash-line (Figure 1). This incision is placed close to the palpebral margin so that oedema of the lower lid above the scar following surgery is avoided.
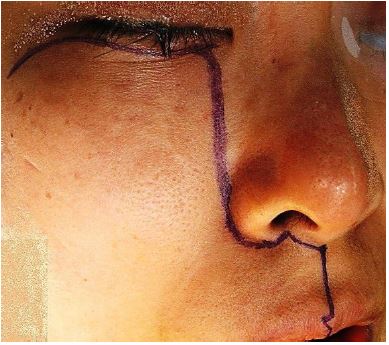
At the vertical or parasagittal plane of the lateral orbital rim, the incision turns posteroinferiorly towards the 135 degree angle that the inferior border of the maxillary process of the zygoma makes with the zygomatic process of the maxilla. This inferior border can be palpated through the soft tissues of the lateral cheek. The incision is marked to the midpoint of this angled line between the lateral orbital rim and the inferior border of the zygoma. It is roughly parallel but posterior to the zygomaticomaxillary suture line (Figure 1).
Unlike the Weber Ferguson incision that follows the concept of facial subunits, the medial end of the lower eyelid incision is not carried onto the nasal bone, but instead avoids the epicanthal fold and so turns inferiorly just before the vertical or parasagittal plane at the medial canthus to follow the junction of the cheek and the lateral nose up to the ala. It then follows the alar groove around and into the nostril. After a 90 degree notch is made on the nasal sill of the floor of the vestibule, the incision then continues to the midline at the junction of the columella and the lip, at which point it turns inferiorly through 90 degrees and continues in the midline of the philtrum to the midline of the upper vermillion border of the lip. A notch is made along this border too and the incision continues in the midline of the lip and through the superior labial frenulum of the buccal surface of the lip to the midline gingiva between the upper central incisors (Figure 1).
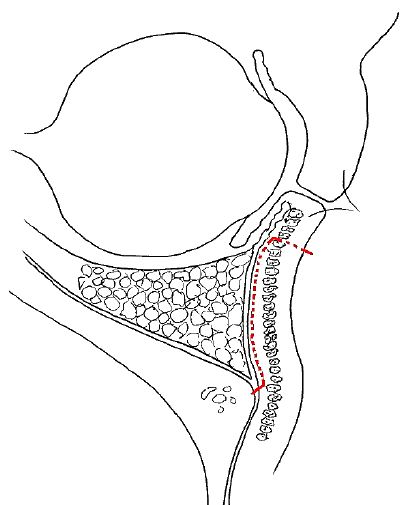
Use a tonsil or Ferguson Auckland mouth gag to open the mouth and retract the tongue to visualize the hard and soft palates. Mark a paramedian or parasagittal incision on the hard palate extending from the junction of the hard and soft palate posteriorly to the premaxillary mucosa anteriorly, 7mm from the midline on the side of the swing. Here the incision then turns towards the midline and to the gingiva between the two upper central incisors Figure 2.
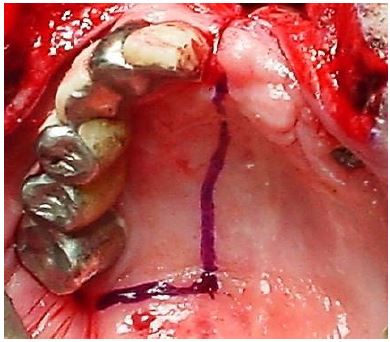
Palpate and identify the maxillary tuberosity and the bony spines of the pterygoid plates and pterygoid hamulus immediately posterior to the tuberosity. The line of the posterior end of the hard palate incision is continued laterally through the mucosa of the soft palate to the posterior aspect of the maxillary tuberosity (Figure 2).
Soft tissue dissection to expose bone for osteotomies
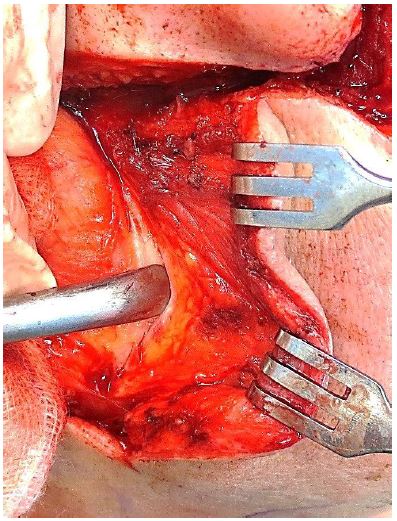
All the incision lines are infiltrated with a vasoconstrictor e.g. 1:80,000 adrenaline. Facial skin incisions are made with a scalpel. Facial and palatal incisions are carried through skin or mucosa to periosteum and bone apart from the incisions in the lower eyelid and soft palate. While applying very gentle pressure to the eye and retracting the skin of the cheek, the lower eyelid is put under tension and the skin is incised with a number 15 scalpel blade (Figure 3).
Figure 3: Lower eyelid is put under gentle tension while incision is made

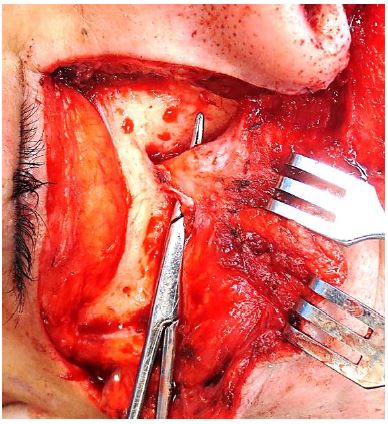
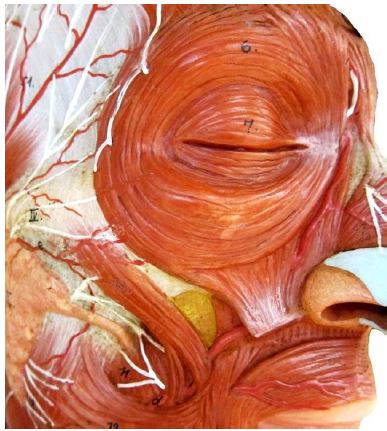
The skin incision is deepened until the stretched orbicularis oculi muscle comes into view. This muscle is gently stroked with the blade until all the fibres are divided taking care not to incise the inferior orbital septum or anterior capsule of the inferior orbital fat pad. Using single skin hooks to retract the skin of the lower eyelid, the skin and orbicularis oculi muscle are elevated as a unit with sharp dissection from the orbital fat pad in a preseptal plane. Using sharp dissection on the septum of the inferior orbital fat pad preserves the facial nerve branches which innervate the orbicularis muscle on its deep surface (Figure 4).
Where the medial end of the lower eyelid incision turns inferiorly, the angular vein and artery are encountered; they are ligated and divided to avoid them retracting and causing troublesome bleeding (Figures 5, 6).

The inferior orbital septum fuses with the periosteum at the superior aspect of the inferior orbital rim. The periosteum of the inferior orbital rim is incised anterior to this line of fusion so as to preserve the integrity of the inferior orbital fat pad (Figure 7).
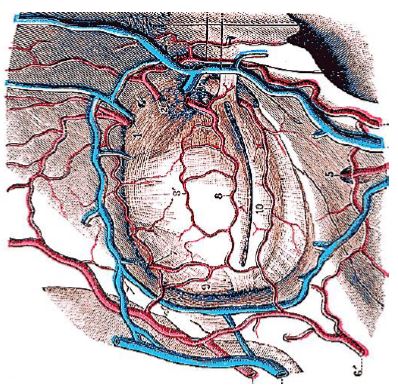
Using a Howarth’s periosteal elevator the soft tissues of the cheek are elevated off the upper maxilla in a subperiosteal plane to the level of the infraorbital foramen (Figure 8). The infraorbital nerve and vessels are identified and ligated and divided (Figure 9).
Do not elevate the soft tissue off the anterior maxilla further inferiorly than the infraorbital foramen as the maxilla depends on the soft tissue of the cheek for its blood supply.
Remain in the subperiosteal plane at the lateral end of the lower eyelid incision while elevating tissue off the zygoma until the inferior margin of the zygoma can be palpated with the angled end of the elevator. It is not necessary to incise the skin over the entire zygoma, but just enough to allow an osteotomy to be made. Usually the skin incision is made up to the midpoint of the zygoma.
Muscles incised with the facial incisions include the orbicularis oculi, nasalis and orbicularis oris (Figure 10).
Next the nasal cavity is entered through the facial wound. Once the rim of the ipsilateral pyriform aperture has been defined, free the soft tissues of the nasal cavity from the free margin of the nasal aperture with diathermy. Retract the nasal ala medially and incise the lateral wall of the nasal vestibule to expose the ipsilateral nasal cavity and inferior turbinate, taking care not to injure the inferior turbinate or septum so as to avoid troublesome bleeding.
At the inferior margin of the aperture, use an elevator to elevate the mucoperiosteum off the floor of the nasal cavity. Elevate the entire mucoperiosteum of the floor of the nasal cavity, from the septum medially to the lateral aspect of the inferior meatus, and from the pyriform aperture anteriorly to the posterior margin of the hard palate posteriorly i.e. the horizontal plate of palatine bone. Then incise the elevated mucosa from anterior to posterior as laterally as possible to create a medially based mucoperiosteal flap that will be used to cover the maxillary osteotomy at the end of the procedure (Figures 11, 12).
Incise the mucosa of the hard palate along the paramedian incision line onto bone with a scalpel. Extend the incision laterally along the soft palate from the posterior edge of the hard palate incision to the groove between the maxillary tuberosity and pterygoid plates (Figure 2). Use a periosteal elevator to elevate the mucoperiosteum of the hard palate off the bone in a subperiosteal plane on the non-swing side of the palatal incision to just across the midline (Figure 12).
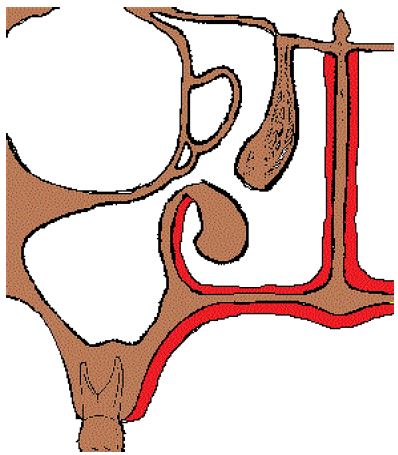
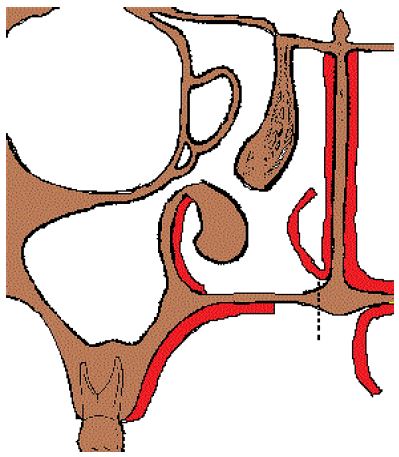
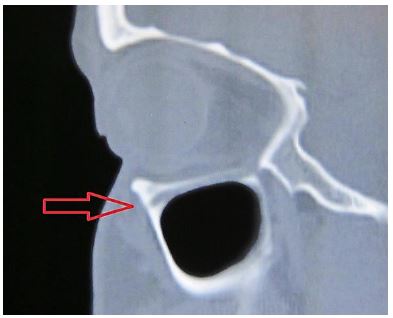
Refer to the patient’s sagittal imaging to confirm that the orbital floor does not dip below the level of the infraorbital foramen in the plane of the foramen, nor at the midpoint of the orbit (Figure 13). If this is the case, then the osteotomy must be placed below the level of the orbital floor.
If the orbital floor does not bulge or hang into the antrum (Figure 14), then a straight horizontal osteotomy is marked at the level of the inferior margin of the infraorbital foramen, from the rim of the pyriform aperture medially to the malar aspect of the zygoma laterally (Figures 15, 16, 17). This osteotomy separates the bony orbit superiorly from the remaining maxilla / zygoma inferiorly.
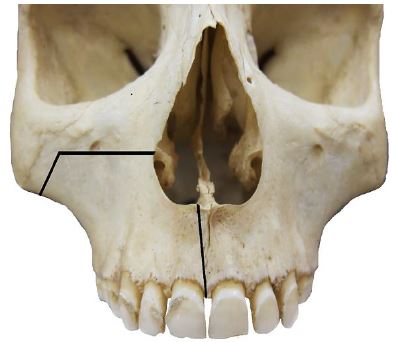
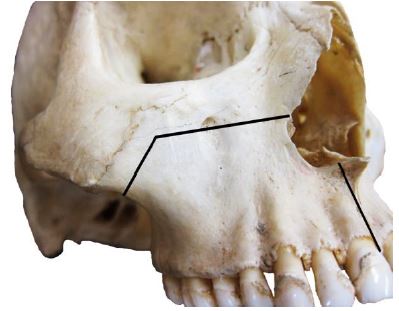

At the lateral end of this osteotomy, a 2nd osteotomy is marked at 90 degrees to the posteroinferior border of the zygoma. This osteotomy will complete the division of the zygoma (Figures 15, 16).
A 3rd osteotomy is marked vertically in the midline of the anterior maxilla and extends between the medial incisors (Figures 15, 16).
On the exposed bone of the hard palate (palatine process of maxilla and horizontal plates of palatine bones), the osteotomy is marked just off the midline on the ipsilateral side so that it divides the floor of the nasal cavity from the nasal septum and is not made through or involves the septum. This osteotomy divides the maxilla just off the midline so that the septum remains intact and articulates with the contralateral maxilla (Figures 12, 15, 24).
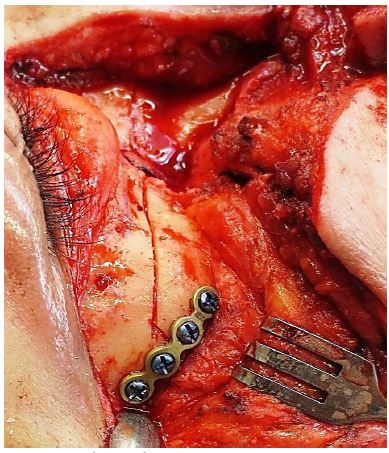
Use a 1x1cm thin sagittal saw to mark the osteotomies before two 4-hole miniplates are fashioned and screw holes are drilled (Figures 18, 19). The miniplates are contoured to the bone. At the osteotomy site in the midline of the anterior maxilla a very prominent bony crest may need to be burred down to accommodate the miniplate (Figures 15, 16, 18). It is important that screw holes avoid the dental roots by positioning the miniplates above or between roots if the height of the maxilla is inadequate (Figure 18). A 2nd miniplate is positioned over the osteotomy made through inferolateral zygoma (Figure 19).
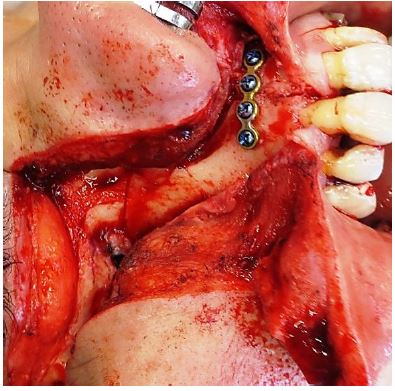
The miniplates should be positioned at 900 to the osteotomy (Figures 18, 19). As each hole is drilled, a screw is inserted but not fully tightened, before drilling the next hole, as drilling all the holes before inserting any screws may cause misalignment. Remove all screws and record or mark in some way the orientation of the plates; it is the author’s preference to make a drawing on paper and use sterile adhesive strips to attach the orientated plates to the diagram.
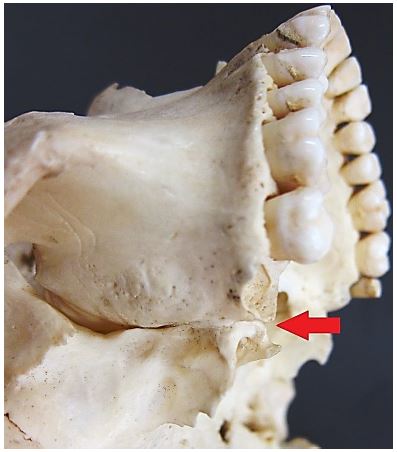
We first do the osteotomy that separates the maxilla from the pterygoid plates as the maxilla is still stable. There is no movement of the maxilla at this stage as the other osteotomies have not yet been done; doing it after the other osteotomies causes unpredictable fracturing of the pterygoid process. This osteotomy is done behind the maxillary tuberosity and frees it from the pterygoid plates. A heavy curved osteotome is passed into the oral cavity with its blade placed in the mucosal incision (Figures 20, 21). With the surgeon guiding the osteotome with a finger, an assistant taps the osteotome to complete the osteotomy. The osteotome traverses the pterygomaxillary fissure and ends in the pterygopalatine fossa.
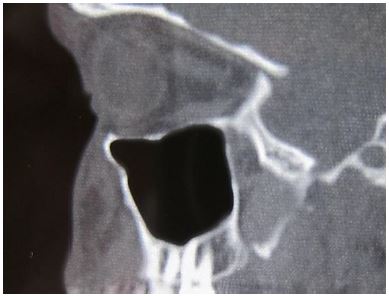
Check the axial CT images and measure the anterior-posterior dimensions of the maxillary sinus to determine the distance from the anterior surface of the maxilla to the posterior wall of the maxillary sinus (Figure 22). Deepen the maxillary and zygomatic osteotomies to the hilt of the more controllable 1cm oscillating saw blade, keeping the blade perpendicular to the bone; then the blade is changed for a longer 4cm blade.
The posterior wall of the maxillary sinus does not need to be cut with a saw as it is thin and fractures easily when the maxilla is mobilised. In fact, sawing through the posterior wall of the antrum should be avoided as it will lacerate the internal maxillary artery and cause significant bleeding before the osteotomies can be completed and the maxilla swung to gain access to the bleeding artery.
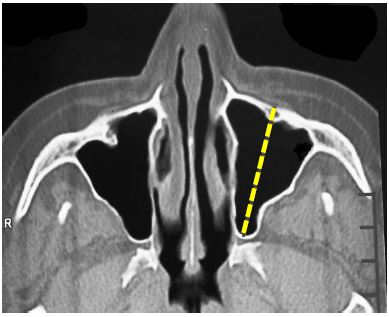
When making the infraorbital osteotomy it is important to keep the blade horizontal. It is especially important to be aware (from the preoperative imaging) of the level of the orbital floor and whether it dips below the infraorbital foramen so as to avoid injuring the contents of the orbit when doing the osteotomy. Medially cut through the lateral nasal wall and laterally, the lateral wall of the antrum.
When making the midline paramedian or parasagittal vertical maxillary osteotomy under direct vision (Figure 23), an assistant ensures that the mucoperiosteal flaps of the hard palate and the nasal floor are retracted away from the blade so as not to damage or lacerate them (Figure 12). The palatal osteotomy is extended posteriorly up to the posterior edge of the hard palate (Figure 23).

Next insert a sharp, straight osteotome into the anterior vertical osteotomy and gently twist it to fracture the remaining bony connections, usually the thin posterior wall of the maxillary antrum (Figures 24, 25).


If the maxilla remains stable, twisting and tapping of a sharp straight osteotome can be done at multiple sites taking care not to damage the screw holes.
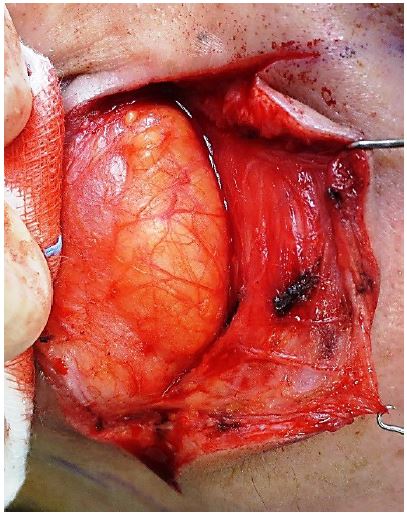
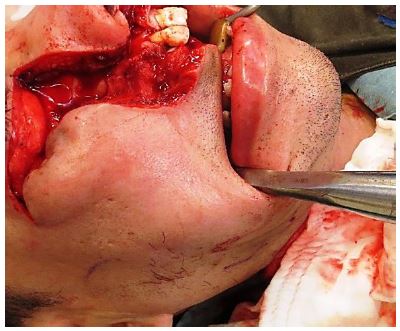
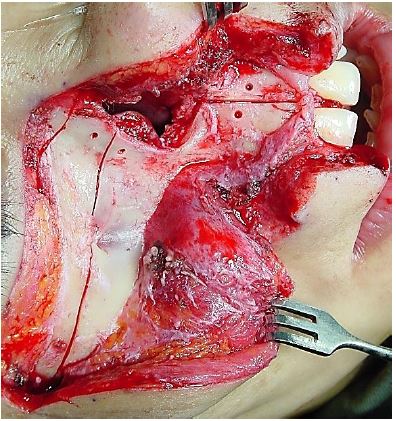
Once the maxilla is loose it is gently retracted / swung laterally / out-fractured. Any soft tissue that tethers the maxilla is divided with a pair of curved Mayo scissors (Figure 27). The maxilla is wrapped in a long length of saline-soaked swab which is used to retract and keep the maxilla out of the surgical field with a Rochester Pean forceps or equivalent.
If significant bleeding occurs, it is usually due to laceration of the internal maxillary artery which must quickly be controlled. Using suction and a long curved haemostat the artery is clamped, divided and tied with a silk ligature.
The inferior turbinate is excised and the posterior nasal septum can be resected for better exposure of the nasopharynx.

Following resection of the nasopharyngeal tumour one can proceed to closure.
Bleeding might occur from the pterygoid venous plexus and is initially controlled with packing. Meticulous haemostasis is achieved with combinations of bipolar cautery, suture ligatures, clips, bone wax, oxidized cellulose polymer and topical haemostatics.
A fine-bore nasogastric feeding tube is inserted through the contralateral nasal cavity for postoperative enteral feeding.
Depending on the type of surgery, the nasopharyngeal wound may be left to mucosalise, or is dressed with a mucosal graft taken from the inferior turbinate, or with a vascularized septal mucosal flap based on the posterior nasal artery.
The nasopharynx is packed with a dressing via the ipsilateral nasal cavity, e.g. a single length of paraffin gauze, to hold grafts in place and to promote mucosalisation.
A Foley catheter is inserted into the nasopharynx via the contralateral nasal cavity and the balloon is inflated with just enough sterile water to prevent the nasal packing from slipping into the oropharynx.
An inferior meatal antrostomy is fashioned in the swung maxilla by carefully elevating the mucosa from the medial wall of the antrum and using a bone nibbler to remove bone. Mucosa is laid over the raw bone. In this way the crest between the nasal cavity floor and antral floor is removed which allows for free drainage of antral mucus.
The soft and hard palate mucosal incisions are preloaded with 3.0 synthetic absorbable polyglycolic acid sutures. This permits accurate suture placement while maximum access is still available. Posteriorly it is best to insert the suture through the mucosa of the soft palate and then through the posterior mucosa of the swung maxilla. Medially it is best to insert sutures through the mucoperiosteum of the swung maxilla and then through the mucoperiosteum of the contralateral hard palate flap. The sutures are kept in order by clamping each with a haemostat and sliding its eye ring or finger grip onto a closed bigger forceps.
The maxilla is reduced and held firmly in position (Figure 27). Ensure that neither the mucosal flap of the nasal floor, nor packing material, is trapped between bony bones.
The two 4-hole miniplates are securely screwed into place while maintaining bony reduction; each screw is tightened but not to the point of stripping either the bone or the threads of the screws (Figures 18, 19).
The sutures of the palatal mucosa are tied, starting posteriorly. This should be done with care as it is not possible to reinsert a suture should it tear out or snap.
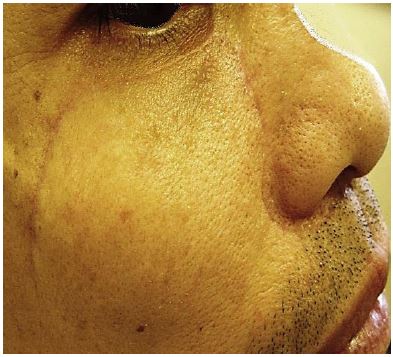
The facial and lip wounds are closed in two layers i.e. a deeper subcutaneous layer and a skin layer. For the subcutaneous layer and for the lip mucosa the author uses a 3.0 braided absorbable suture, and for the skin a 4.0 non-absorbable monofilament suture, except for the lower eyelid where a 5.0 suture is used.
It is important to securely anchor the superomedial corner of the cheek flap to avoid the tension on the cheek flap being transmitted to the lower eyelid wound; this is achieved by preloading four braided absorbable sutures deeply with sufficient tissue on both sides of the wound before tying the sutures and closing the rest of the wound of the cheek and eyelid.
A prefabricated palatal dental splint is securely placed to maintain apposition of the hard palate mucoperiosteal flap against the underlying bone during the healing phase.
Figure 28 demonstrates a patient at conclusion of surgery. Note the tracheostomy tube; fine-bore feeding tube in the contralateral nostril; and a Foley catheter with cuff inflated to prevent packing falling into the oropharynx.

Day 0: Perioperative antibiotics are continued for 5 days; chest x-ray is done to confirm the position of the nasogastric tube prior to feeding; chest physiotherapy; tracheostomy care; mouth care; and routine postoperative blood tests
Day 1: Foley catheter in nasopharynx deflated after 24 hours
Day 5: Lower eyelid sutures removed
Day 6: Nasopharyngeal pack loosened and shortened
Day 7: Nasopharyngeal pack removed; start rinsing nasal cavities and nasopharynx three times/day with normal saline; rest of facial sutures removed
Day 8: Tracheostomy tube removed if there has not been significant bleeding
Day 14: Nasogastric tube removed and oral liquid diet commenced
Day 21: Soft diet commenced if palatal wounds well healed
Lex AC Vlantis MBBCh, FCORL
Associate Professor
Department of Otorhinolaryngology, Head and Neck Surgery
The Chinese University of Hong Kong
Prince of Wales Hospital
Hong Kong SAR, China
lexvlantis@cuhk.edu.hk
Johan Fagan MBChB, FCORL, MMed
Professor and Chairman
Division of Otolaryngology
University of Cape Town
Cape Town
South Africa
johannes.fagan@uct.ac.za