Cancers of the tongue are generally treated with primary surgical resection. Adjuvant irradiation is indicated inter alia for advanced tumours, tumours with perineural invasion (PNI) or uncertain/close margins.
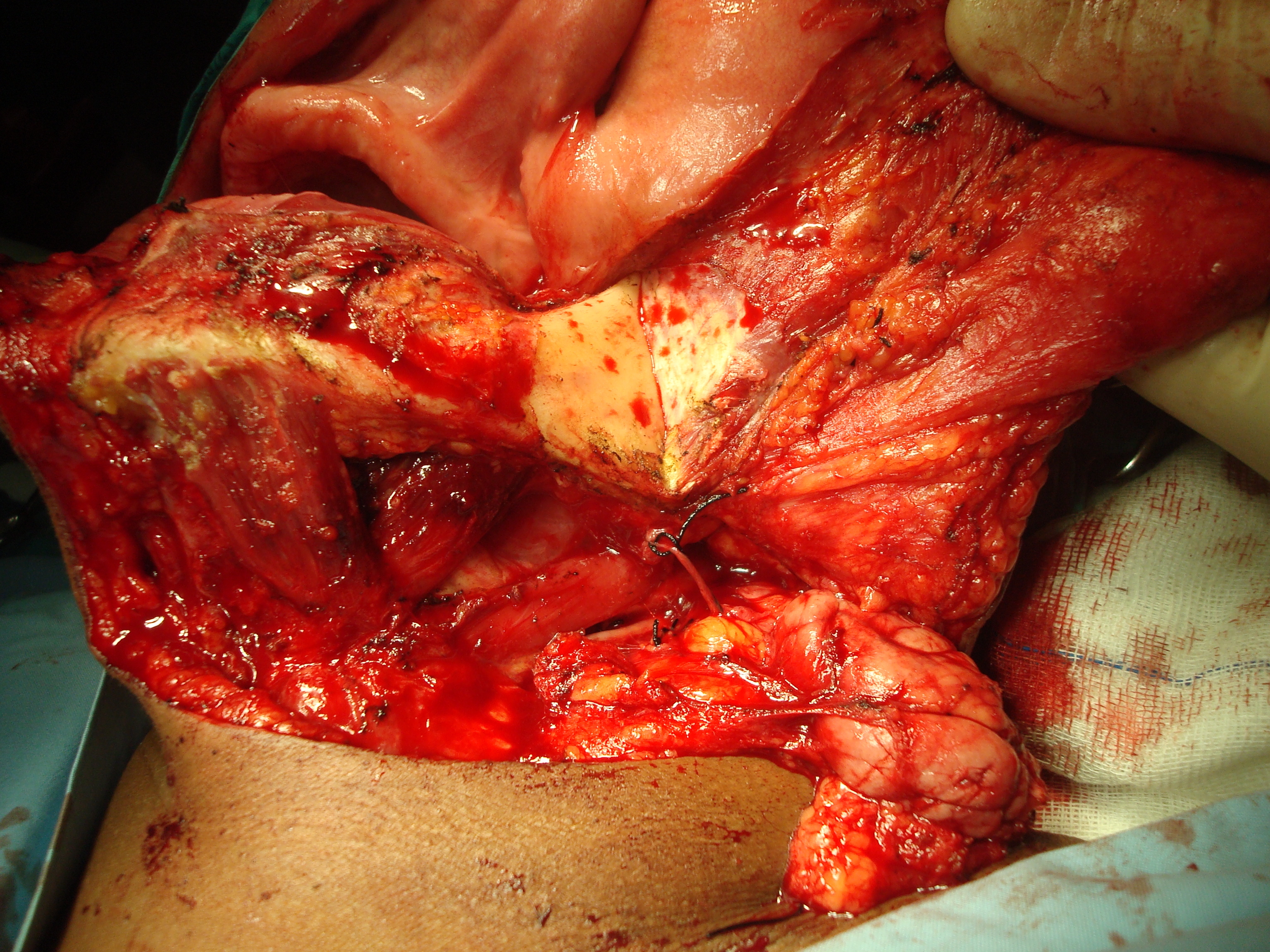
Resecting tongue cancer without con
sidering subsequent oral function may
severely cripple a patient in terms of speech, mastication, oral
transport and swallowing. Resecting the anterior arch of the mandible
beyond the midline without reconstructing bone and with loss of the
anterior attachments of the suprahyoid muscles (digastric, geniohyoid,
mylohyoid, genioglossus) leads to an Andy Gump deformity with loss of oral competence, drooling, and a very poor cosmetic outcome (Figure 1).
The tongue merges anteriorly and laterally with the floor of mouth (FOM),
a horseshoe-shaped area that is confined peripherally by the inner
aspect (lingual surface) of the mandible. Anteriorly the undersurface
of the tongue and FOM has
a covering of delicate oral mucosa through which the thin walled sublingual/ranine veins are visible. The frenulum is a mucosal fold that extends along the midline between the openings of the submandibular ducts towards the tip of the tongue (Figure 2).

Posterolaterally the tonsillolingual sulcus separates the tongue from the tonsil fossa. Posteriorly the vallecula separates the base of tongue from the lingual surface of the epiglottis.
The mucous membrane covering the tongue and FOM varies in thickness and quality; this has relevance in terms of obtaining surgical margins and retaining tongue mobility. The undersurface of the tongue has a thin, smooth, pliable mucous membrane. The mucous membrane covering the anterior 2/3rds of the dorsum is thin and quite smooth and adherent to the tongue muscle compared to the mucosa covering the base of tongue (BOT) behind foramen caecum and sulcus terminalis which is rough, thick and fixed to the underlying muscle and contains a number of lymphoid follicles (lingual tonsil). With BOT tumours it is therefore difficult to determine the edge of a tumour making frozen section especially useful to assess resection margins.
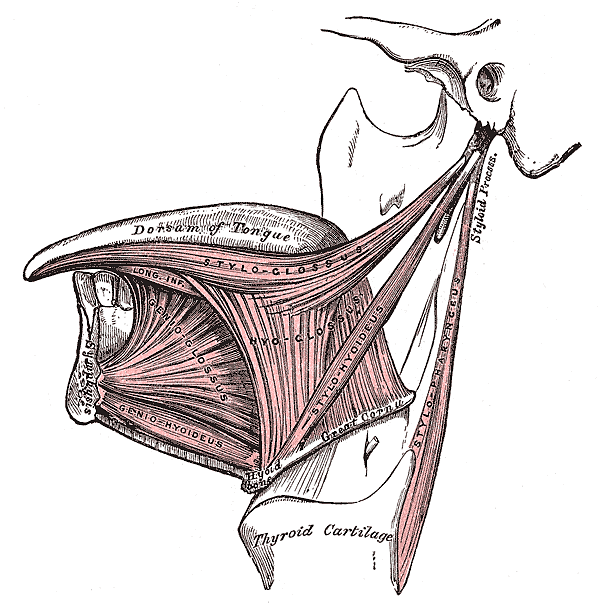
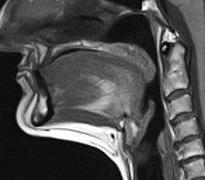
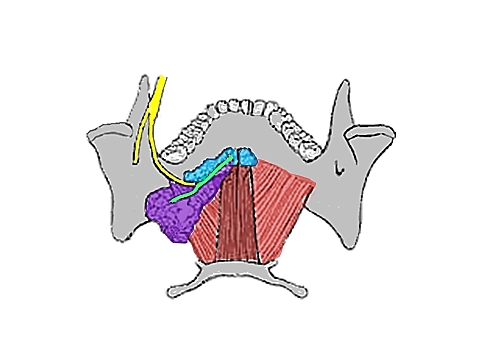
The tongue comprises eight muscles. Four extrinsic muscles (genioglossus, hyoglos-sus, styloglossus, palatoglossus) control the position of the tongue and are attached to bone (Figure 3, 4); four intrinsic muscles modulate the shape of the tongue, and are not attached to bone. Below the tongue are the geniohyoid and the mylohoid muscles; the mylohyoid muscle serves as the diaphragm of the mouth and separates the tongue and FOM from the submental and submandibular triangles of the neck (Figures 3, 4, 5).
The tongue is a very vascular organ. The arterial supply is derived from the paired lingual arteries and its branches (ranine artery, dorsalis linguae, and sublingual arteries) (Figures 6, 7); and the mylohyoid and submental arteries. Additional blood supply to the tongue emanates from the tonsillar branch of the facial artery and the ascending pharyngeal artery.

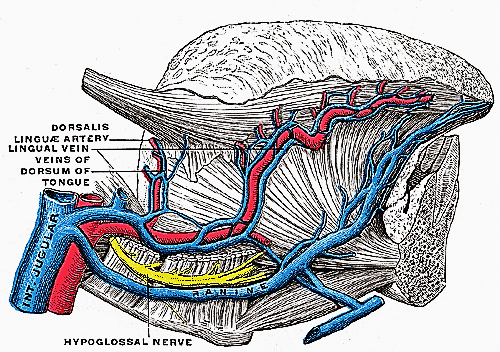
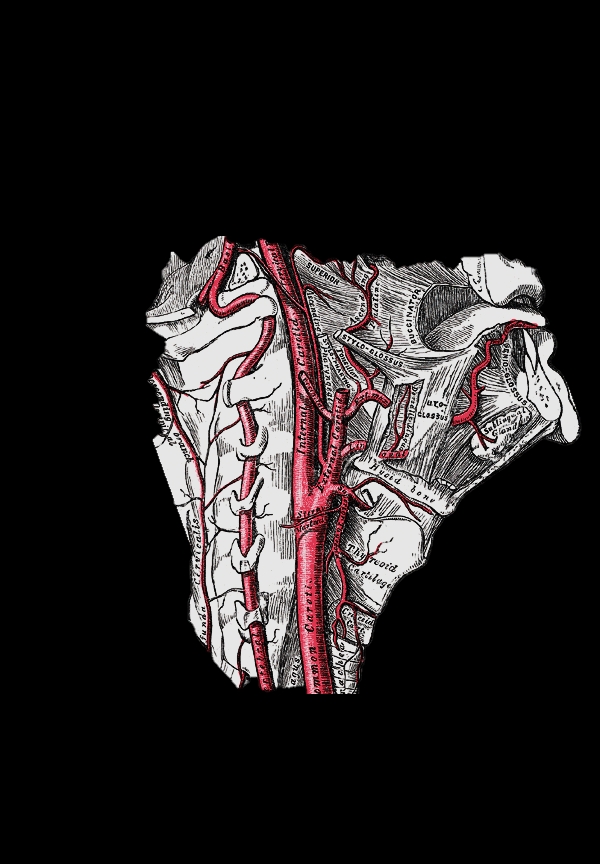
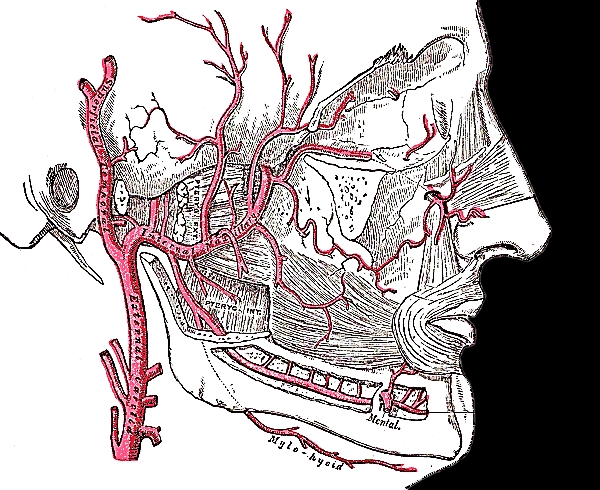
The lingual artery originates from the external carotid between the superior thyroid and facial arteries and courses obliquely forwards and medial to the greater cornu of the hyoid (Figures 6, 7). It then loops downward and anteriorly and passes medial to hypoglossal nerve (XIIn) and the stylohyoid muscle. It then courses directly anteriorly and deep to the hyoglossus and finally ascends submucosally on the undersurface of the tongue as far as its tip as the ranine artery (profunda linguae); it lies to either side of the genioglossus, and is accompanied by the lingual nerve. Two or three small dorsales linguæ arteries arise beneath the hyoglossus and ascend to the posterior part of the dorsum of the tongue and also supply the mucous membrane of the posterior FOM, and oropharynx (Figure 7). The sublingual artery branches from the lingual artery at the anterior edge of the hyoglossus and runs forward between the genioglossus and mylohyoid and supplies the sublingual salivary gland and mucous membrane of the FOM and gingiva (Figure 7). A branch of the sublingual artery pierces the mylohyoid muscle and anastomoses with the submental branch of the facial artery in Level 1b of the neck. The submental branch of the facial artery courses along the inferior, inner margin of the mandible (Figure 8). The mylohyoid artery and vein are encountered when the surgeon elevates the submandibular gland from the lateral surface of the mylohyoid (Figures 8, 9). It branches off the inferior alveolar artery just before it enters the mandibular foramen, crosses the mylohyoid, and disappears anteriorly behind the digastric. It has connections with the sub-mental artery and via a defect in the mylohyoid with the sublingual artery in the FOM.
Venous drainage is via lingual and ranine veins. The lingual veins originate on the dorsum, sides, and undersurface of the tongue and accompany the lingual artery and joins the internal jugular vein. The ranine veins originate below the tip of the tongue and are visible on its ventral surface; they accompany the XIIn as venae comitantes and either join the lingual vein or pass lateral to hyoglossus to join the common facial vein (Figures 2, 6).
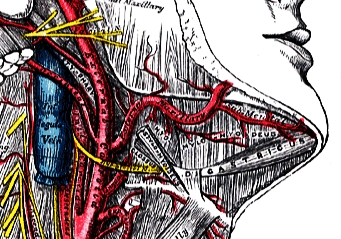
Other than palatoglossus which is innerveted by the Xn, all intrinsic and extrinsic muscles are innervated by the XIIn. The IXn provides somatic afferent and taste sensation to the posterior 1/3 of the tongue. The lingual nerve provides general somatic sensation to the anterior 2/3 of the mouth and FOM; taste is provided by the chorda tympani branch of the VIIn via the lingual nerve. The lingual nerve crosses deep to the submandibular duct in the lateral floor of mouth (Figures 10, 11). In the anterior FOM it is located posterior to the duct (Figure 11).
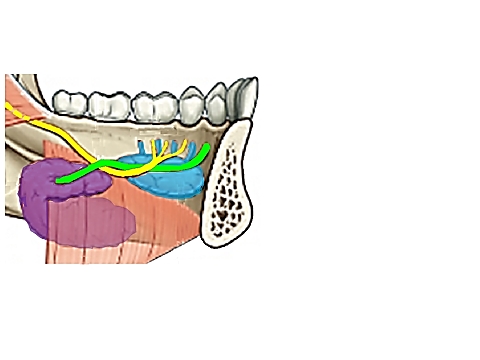
The following structures are located between the mucosa and the mylohyoid muscles: paired geniohyoid muscles in the midline (Figure 4); sublingual salivary glands (Figures 10, 11), submandibular ducts (Figures 10, 11), oral component of submandibular salivary glands (Figures 10, 11), and the lingual and XIIns. The paired sublingual salivary glands are located beneath the mucosa of the anterior floor of mouth, anterior to the subman-dibular ducts and above the mylohyoid and geniohyoid muscles (Figures 10, 11). The submandibular duct is located immediately deep to the mucosa of the anterior and lateral FOM, and opens into the oral cavity to either side of the frenulum (Figures 2, 10, 11).
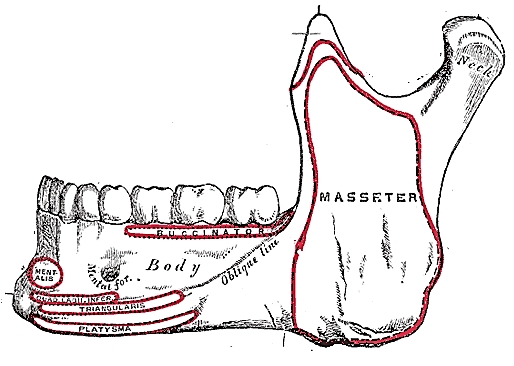
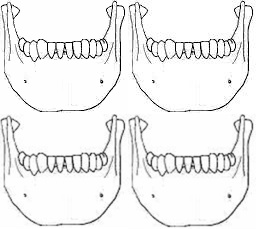
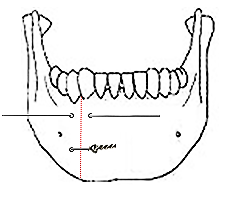
The mandible borders the FOM, and may have to be divided for access (mandibu-lotomy), or resected if involved by tumour (alveolectomy / marginal mandibulectomy / segmental mandibulectomy / hemimandi-bulectomy). Important surgical features are the position of the mental foramina through which the mental nerves exit to innervate the lower lip; the mylohyoid line to which the mylohyoid muscles attach, the attachment of the genioglossus, and when planning marginal mandibulectomy, the height of the body of the mandible and the depths of the dental roots (Figures 12a, b).
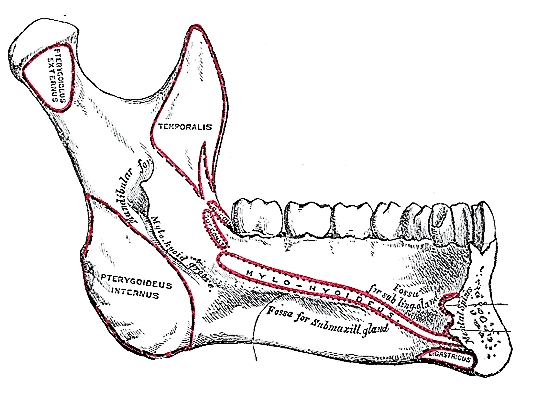
In older, edentulous patients the mandible resorbs and the mental foramen and inferior alveolar nerve may be very close to its superior surface (Figure 13). Marginal mandibulectomy may also not be possible in such a resorbed mandible due to the lack of residual bone.

Surgical Objectives
The author advocates elective neck dissection (END) Levels I-IV for squamous cell carcinoma of the oral tongue that is >4mm thick and/or >T2 stage; a useful rule of thumb is that a tumour which is clinically palpable is likely to have a tumour thickness that warrants END. BOT cancers and tumours of the anterior FOM that approach the midline require bilateral END.
The remainder of this chapter will focus on the surgery of cancer of the oral tongue.
The surgeon should always stand by during induction of anaesthesia as it may be difficult or impossible to intubate the patient, especially with bulky tumours that involve the BOT and preclude elevation of the tongue to visualise the larynx. Should the anaesthetist be unable to intubate the larynx, the surgeon may be able to intubate through a laryngoscope, or do an emergency tracheostomy or cricothyroidotomy. Nasal intubation facilitates resection of tongue tumours, and may be followed by tracheostomy during the course of the operation.
Perioperative antibiotics are prescribed for 24hrs.
Good surgical access is essential in order to attain adequate resection margins, to control bleeding, and for reconstruction.
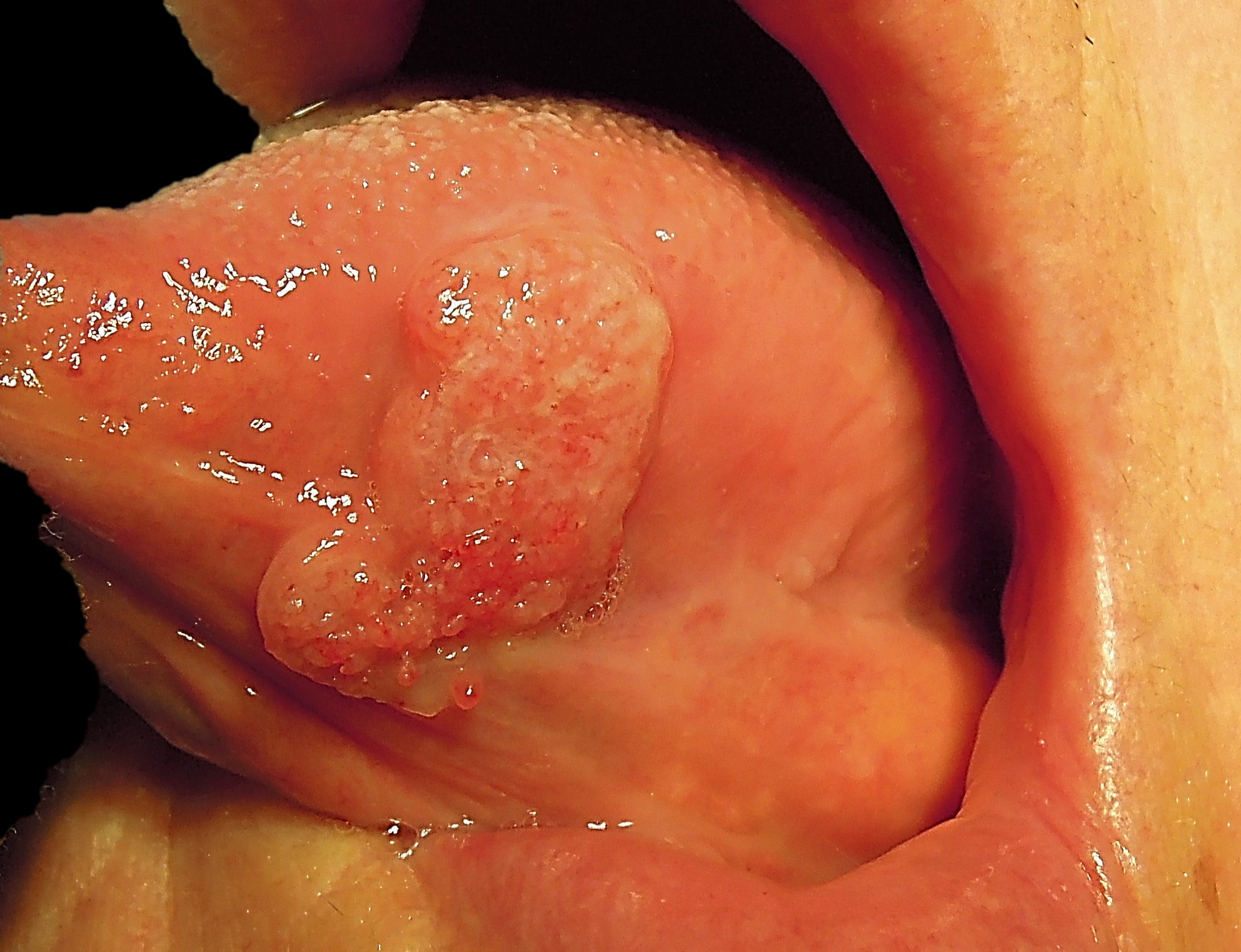
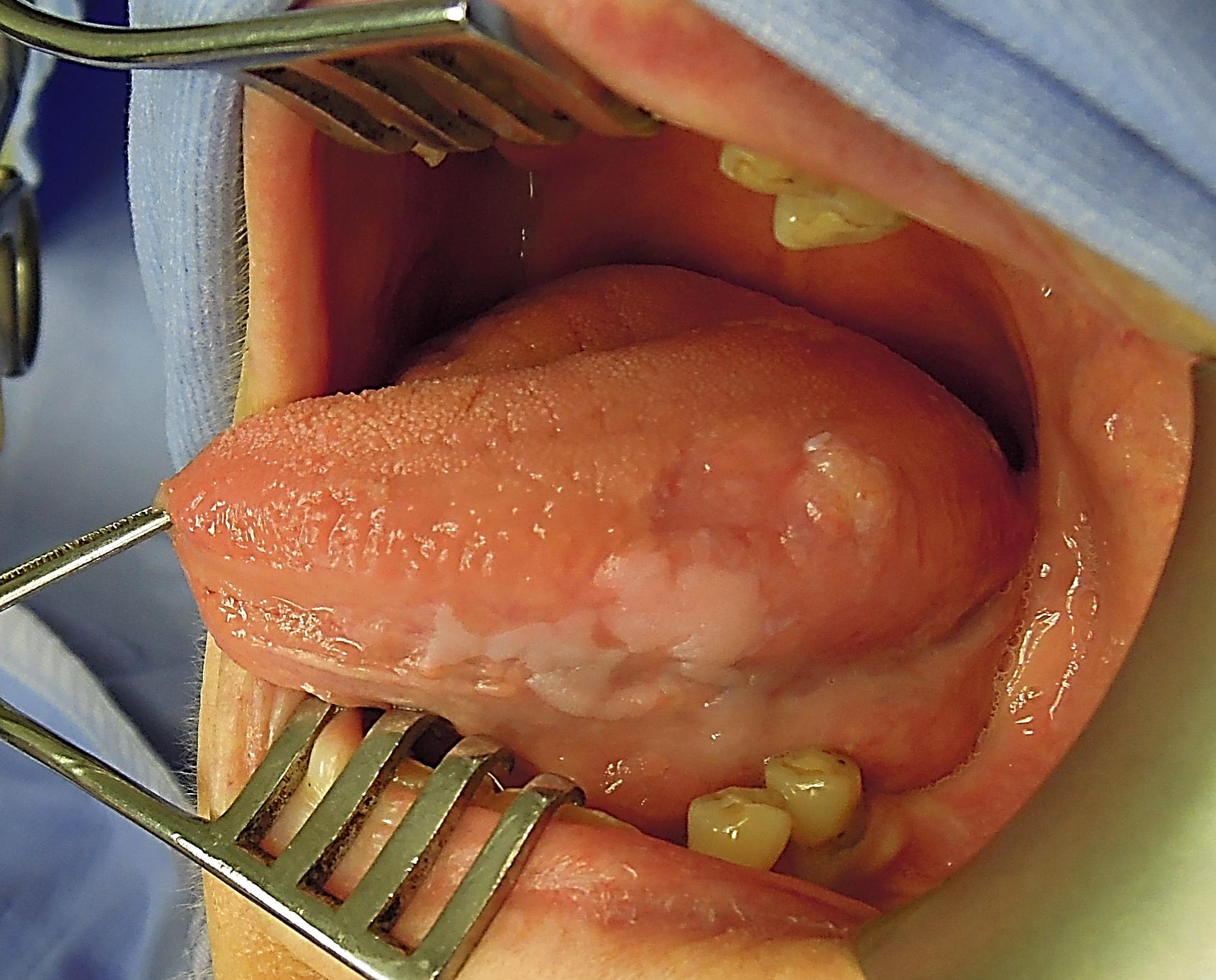
Transoral access: Smaller tumours (T1-T2) are usually easily excised through the open mouth, especially in edentulous patients. The mouth is kept widely open either with a dental bite block (Figure 14) or with a self-retaining retractor, taking care to protect the teeth (Figure 15). First doing the marginal mandibulectomy when tumour abuts the mandible greatly facilitates the resection.
Midline lip-split: The lower lip is vertically divided in the midline after scoring/marking the vermillion border so as to ensure an accurate repair of the lip (Figure 16).
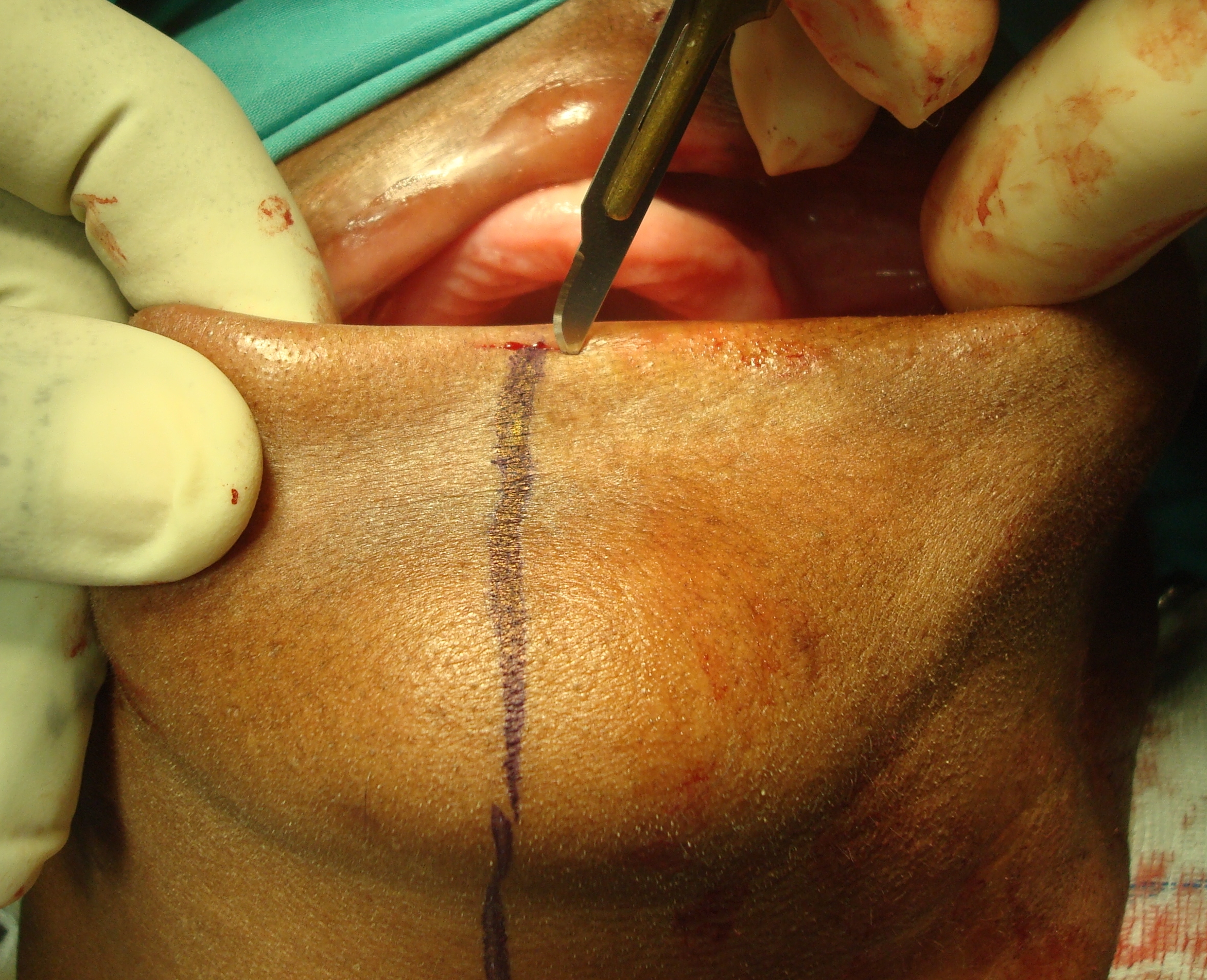
Bleeding from the labial artery is controlled with cautery. Incise the gingivolabial and gingivobuccal mucosa >0.5cms from the bone to facilitate subsequent soft tissue closure. Strip soft tissue off the mandible with monopolar cautery taking care (if possible) not to injure the mental nerve where it exits the mental foramen (Figure 17). Should the mandible need to be resected beyond the mental foramen, then the nerve is divided and the tissues stripped from the lateral surface of the bone (Figure 18).
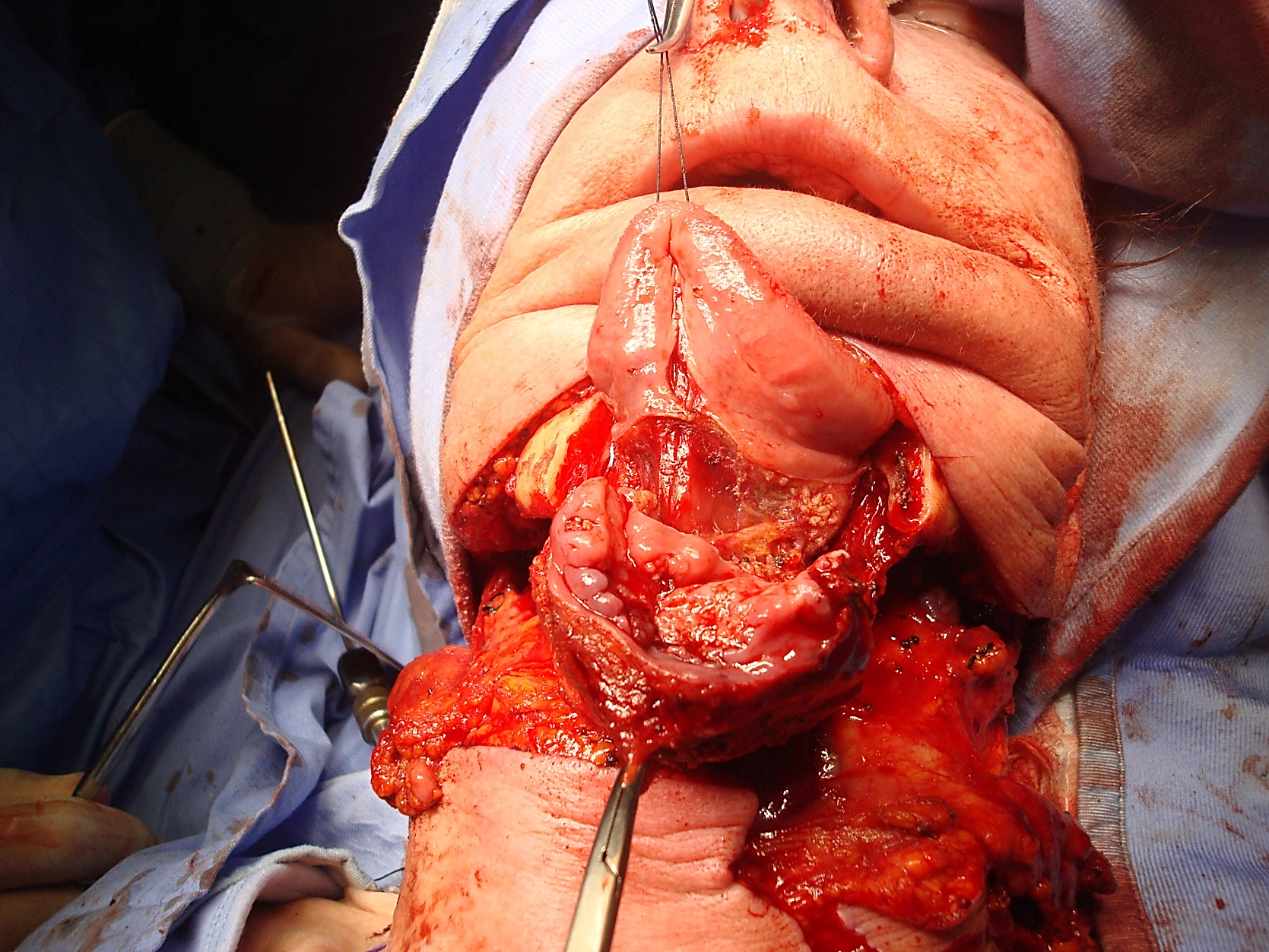
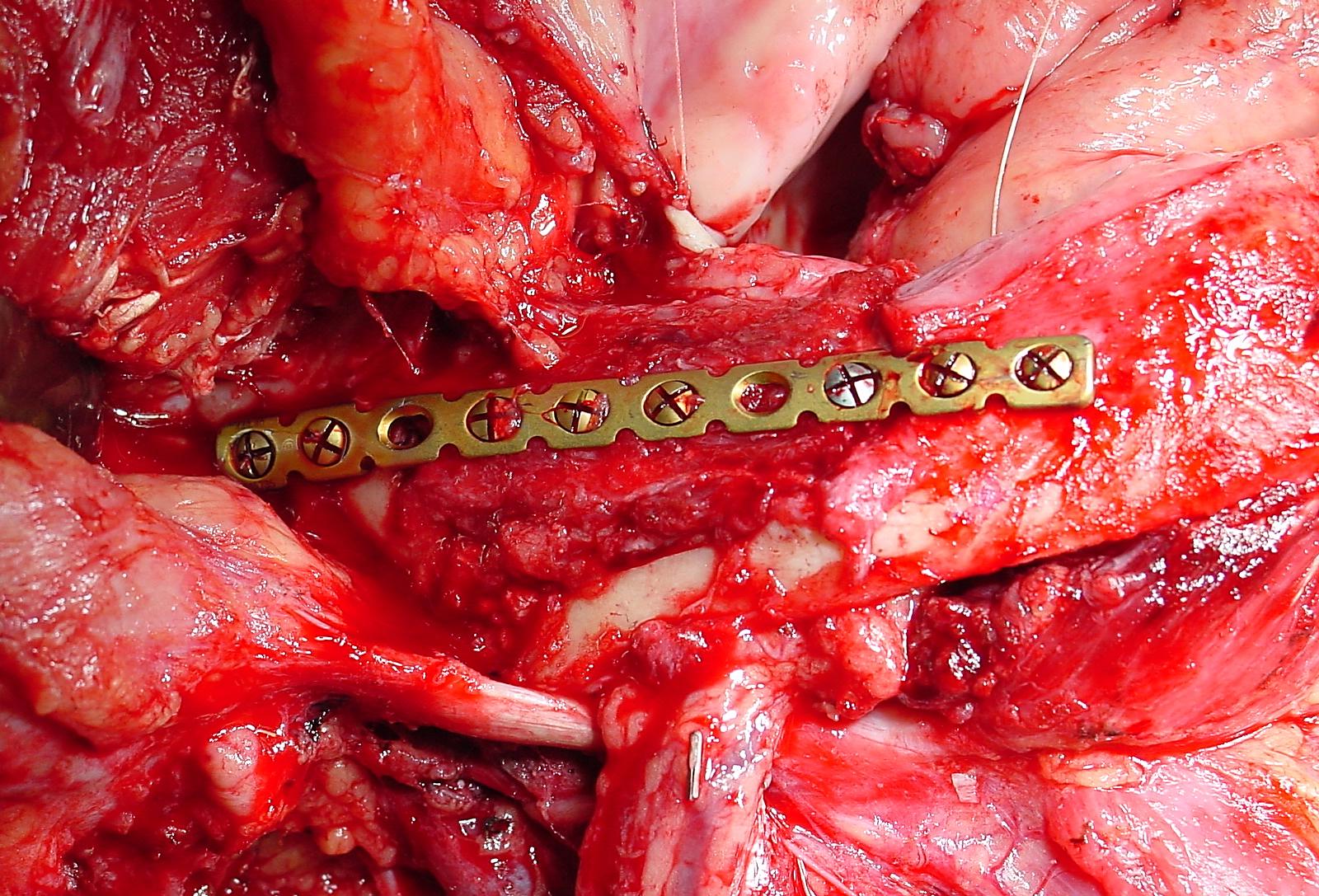
Mandibulotomy: Dividing the mandible following a midline lip-split affords excellent access to the oral cavity with minimal attendant morbidity. The mandible is divided with a Gigli saw (Figure 19) or a powered saw. The osteotomy may be made either vertically or alternatively in a step- or V-shaped fashion so as achieve a more stable repair. The author places the osteotomy just anterior to the mental foramen in lateral tongue cancers (Figure 20). Gigli saws make wider cuts than powered saws; hence it is advisable to extract a tooth and make the osteotomy through the dental socket so as avoid devitalising both adjacent teeth. In dentate patients the mandible is preplated so as to ensure perfect dental alignment.

When plating sets are not available, the mandible is wired together at conclusion of surgery with stainless steel wiring by drilling opposing holes on either side of the osteotomy (Figure 21).
Visor flap: This is achieved by cutting along the gingivolabial and gingivobuccal sulci about 0.5cm from the bone so as to permit placement of sutures when closing the wound, and then stripping the soft tissues from the outer aspect of the mandible. Take care not to transect the mental nerves if they can be saved. The skin flap is then retracted superiorly to expose the mandible (Figure 22).
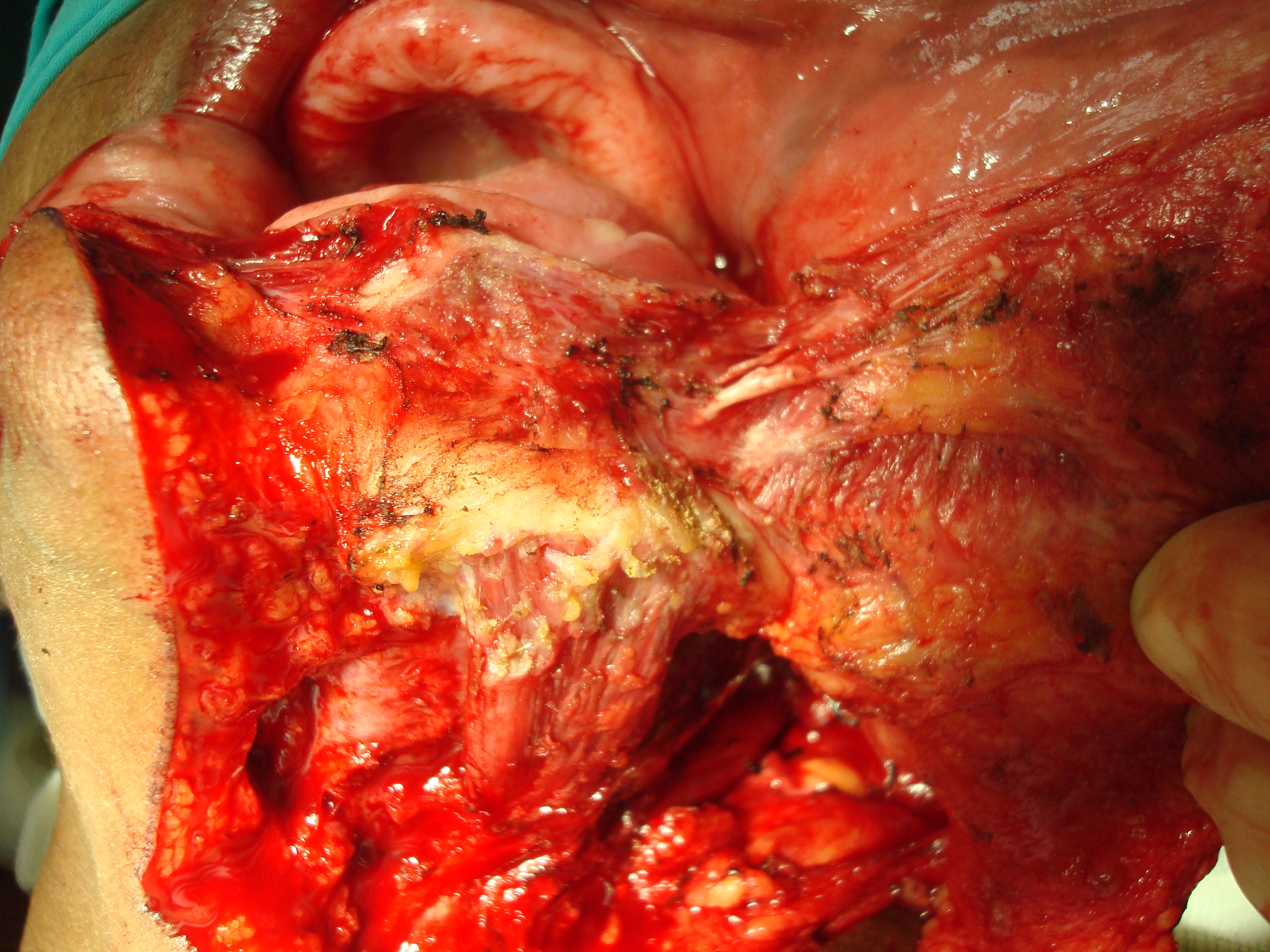
Pull-through: This may be employed when the tumour stops some distance from the inner aspect of the mandible. Following bilateral neck dissections of Levels 1a and 1b, the mandibular attachments of the anterior bellies of digastric, mylohyoid, geniohyoids and genioglossus are divided with electrocautery working from inferiorly. The mucosa of the FOM adjacent to the tongue tumour is then divided >0.5cm from the inner aspect of the mandible (so as to facilitate later repair), taking care not to injure the lingual and XIIns, or the submandibular ducts. This permits the surgeon to deliver the FOM and tongue into the neck and to proceed with the resection.
Having secured surgical access one can proceed to resect the cancer. Complete Levels 1a and b of the neck dissection(s) before proceeding to the resection; this permits the surgeon to cut through the muscles in the FOM and tongue knowing the location of the XIIn, lingual nerve and lingual artery.
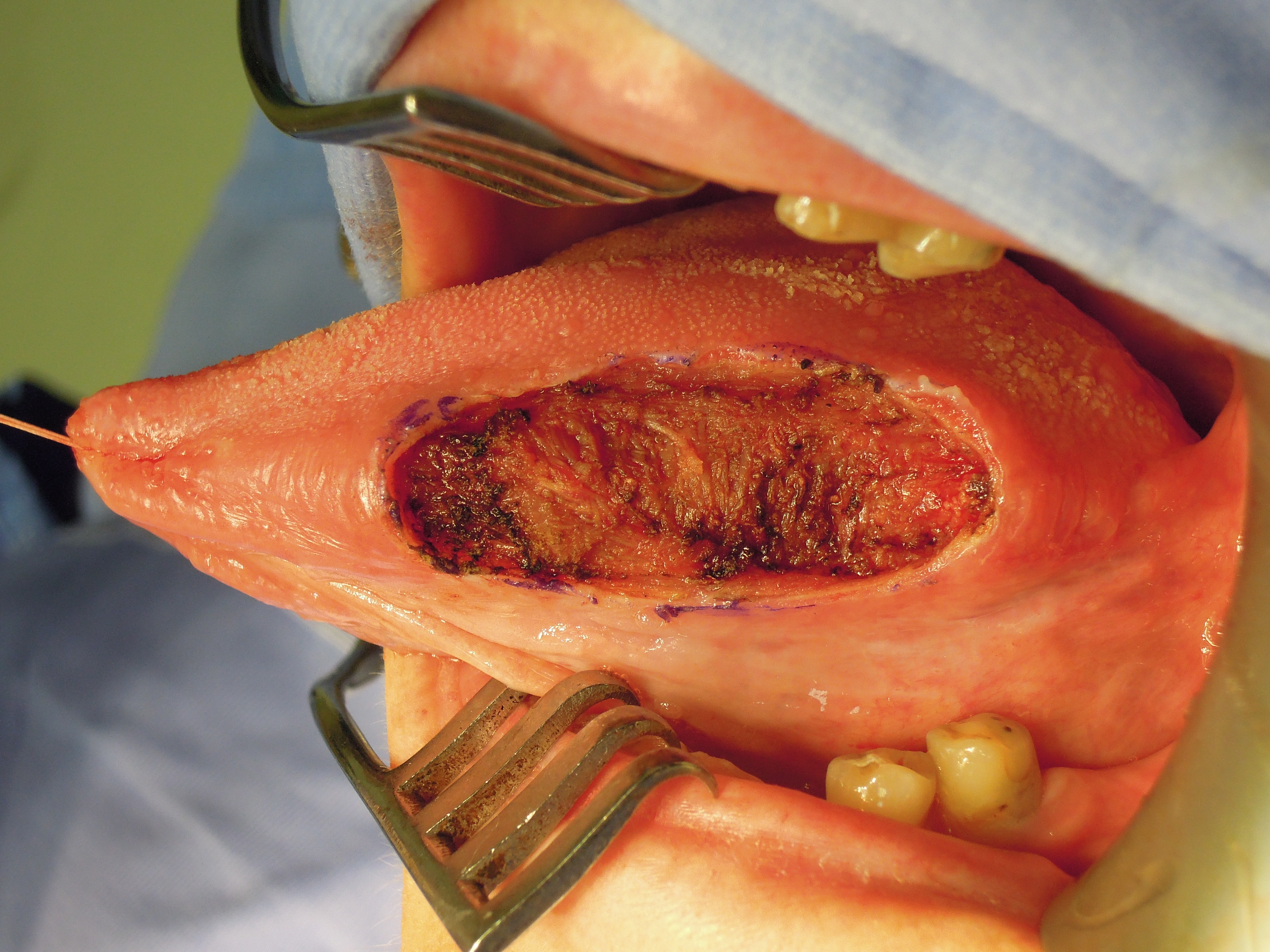
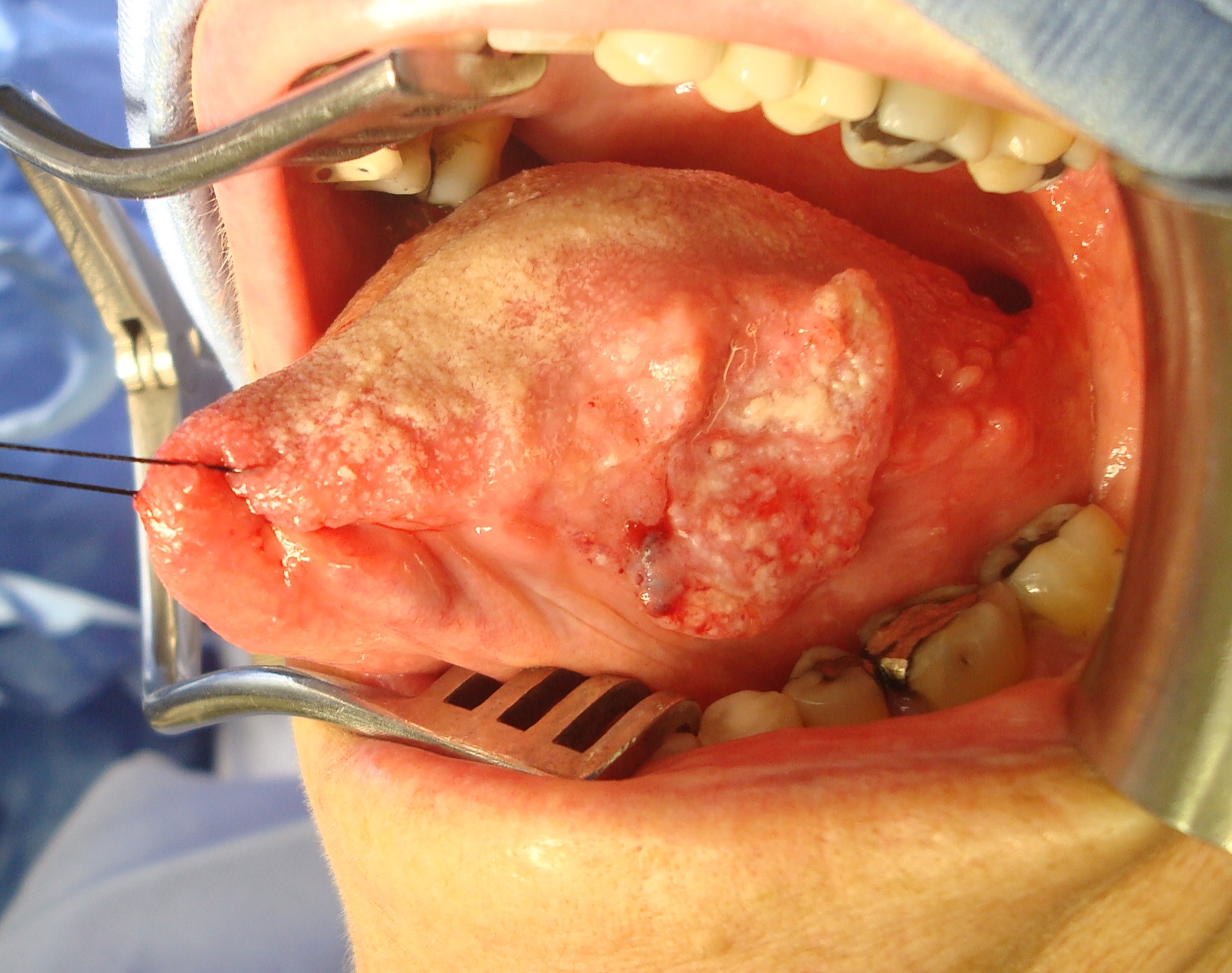
A silk stay suture is placed anterior and/or medial to the tumour to retract the normal tongue (Figure 24b). Use diathermy to resect the tumour with at least 1cm margins. Palpate the tumour repeatedly during the course of the resection to ensure that the margins are adequate. Retain as much FOM mucosa as possible to preserve tongue mobility (Figure 23).
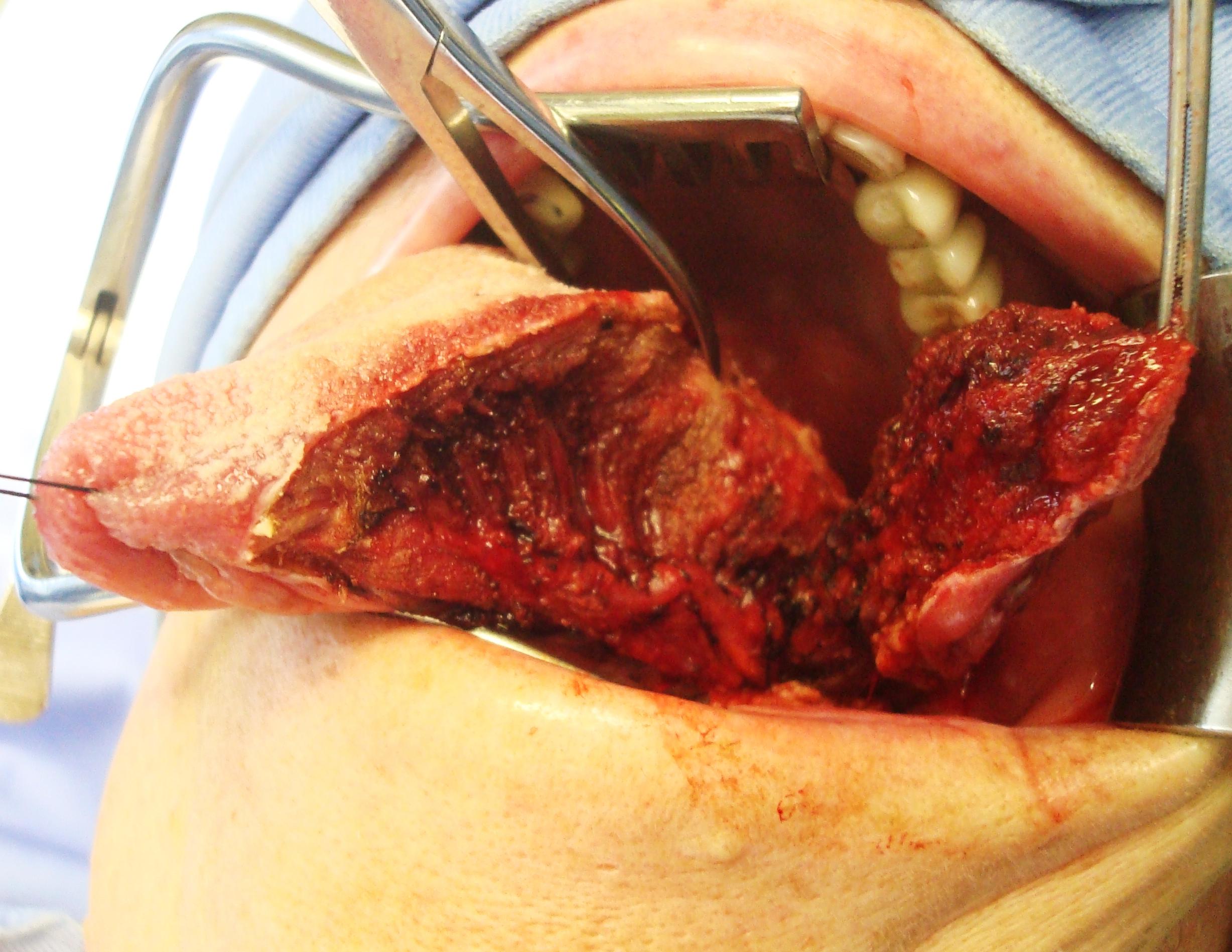
Maintain haemostasis throughout the resection; cauterise the ranine vessels and ligate the lingual artery with silk when it is encountered. Obtain frozen section confirmation of clear tumour margins if available. Orientate the specimen for the pathologist with a suture before removing the specimen so as to not lose orientation.
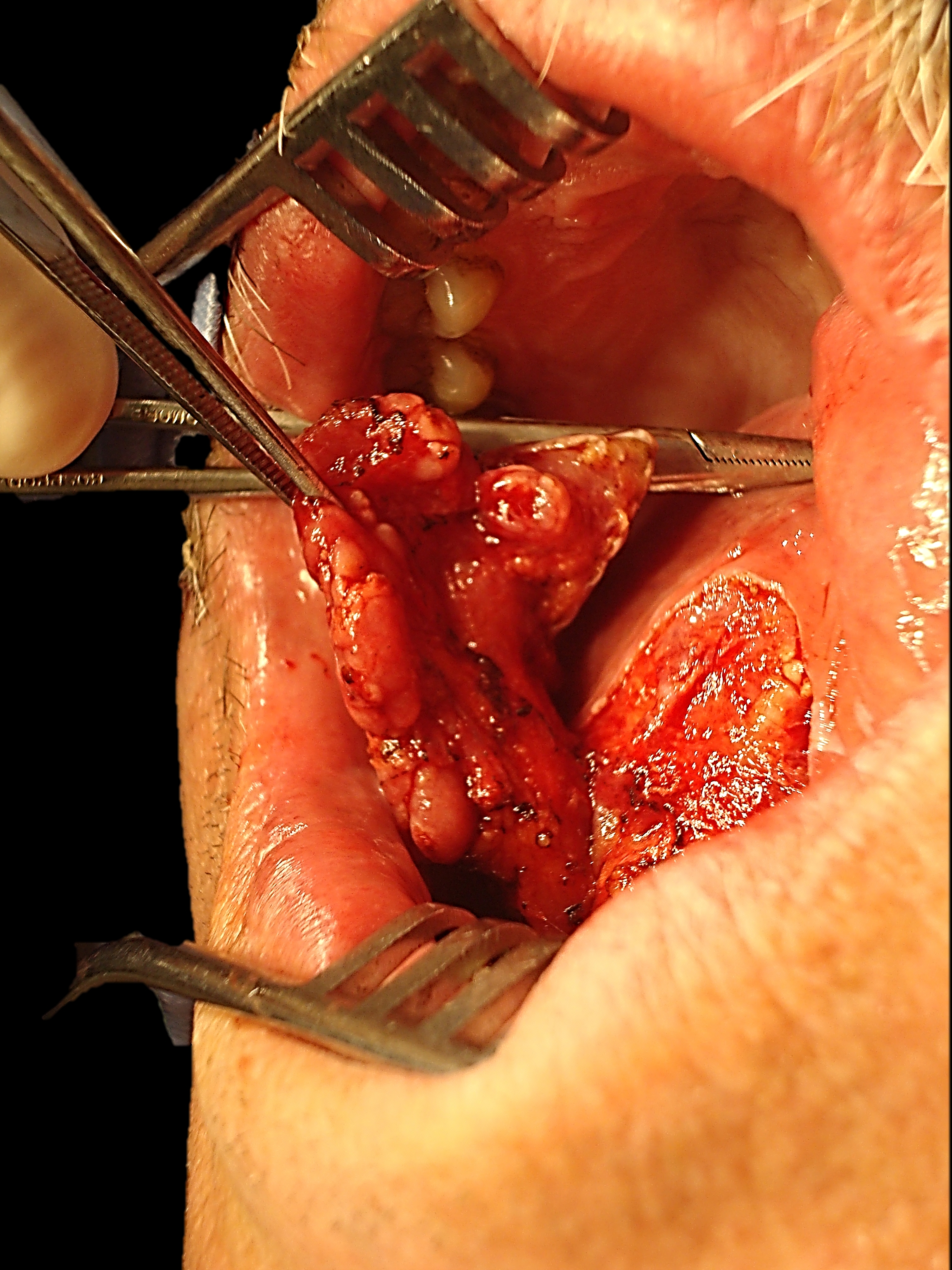
If a marginal or segmental mandibulectomy is required then it should be done before proceeding to partial glossectomy as it improves surgical exposure. Marginal mandibulectomy is done with a powered oscillating or reciprocating saw; or with small sharp osteotomes so as to avoid inadvertently fracturing the mandible. With marginal mandibulectomy the cut is made obliquely so as to remove the inner cortex (including the mylohyoid line) that abuts the tumour but to preserve the height of the outer cortex for mandibular strength. If a segmental mandibulectomy is to be done, then preplate the mandible with a reconstructtion plate so as to ensure alignment of the teeth and a good bony contour. Bone cuts are made at least 2cm from visible tumour. Once the mandibulectomy has been completed, keep the bone attached to the tumour specimen and divide the gingival mucosa on the inside of the bone cuts; this releases tumour from bone and facilitates delivery of the tumour into the surgical field. Identify and preserve the submandibular duct(s), and the lingual and XIIns if possible. The sublingual gland may be encountered in anterior FOM cancer resections.
Repair / Reconstruction
Obtain meticulous haemostasis using ties, monopolar and bipolar cautery before closing the tongue defect. Carefully assess the defect to determine how best to restore form and function i.e. mandibular integrity and contour, oral competence, mastication, oral transport, swallowing and speech.
No repair: Small and/or superficial resections above the mylohyoid that do not communicate with the neck dissection may be left open to heal like a tonsillectomy wound. Resist the temptation to suture such defects as it may alter the shape of the tongue or tether the tongue.
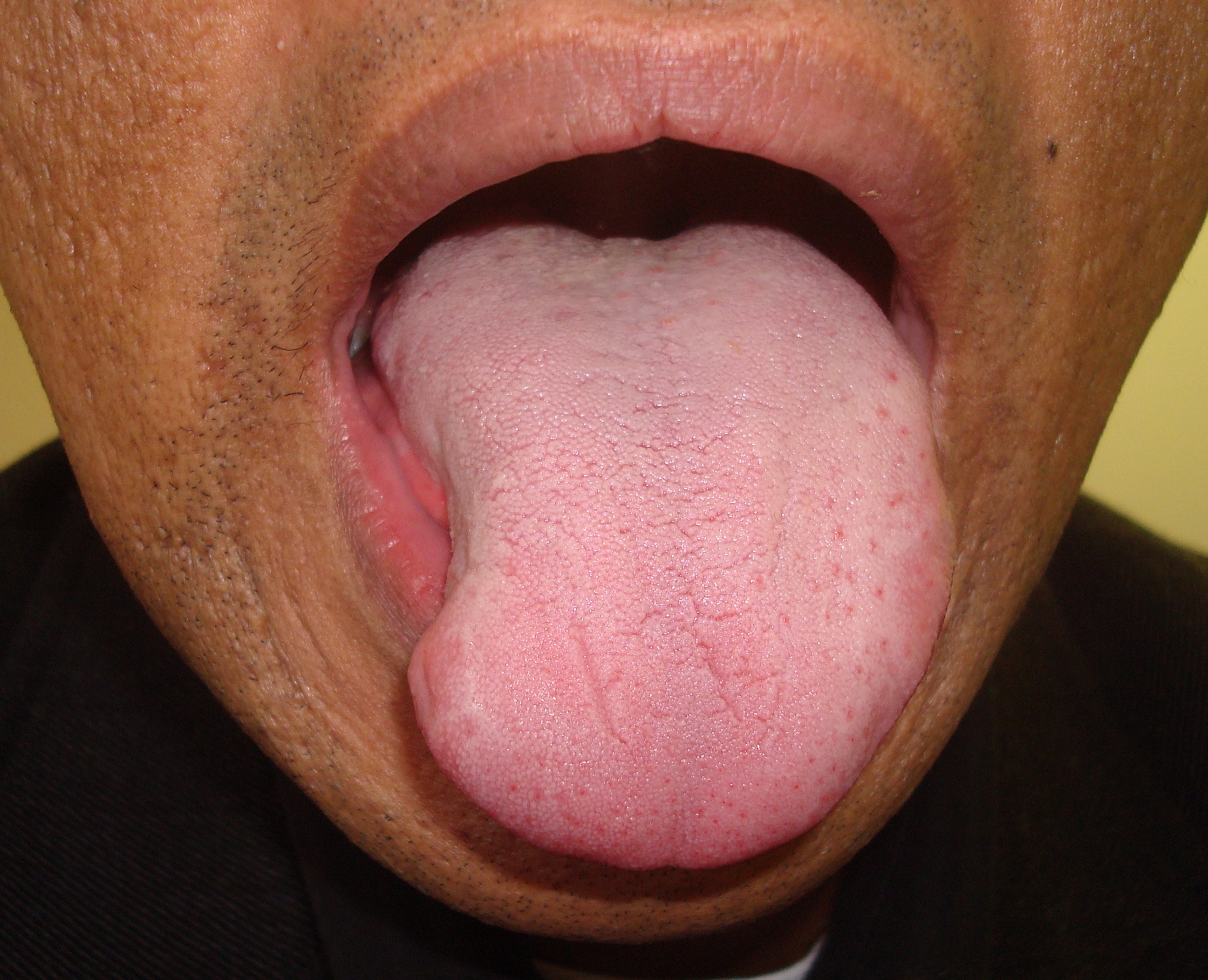
Primary closure (Figure 24a-c): Avoid tethering or distorting the tongue and creating a shortened, stumpy tongue. Preserving FOM mucosa is key to retaining tongue mobility (Figures 25a,b & 26a-c).



Split skin graft: There is little point in grafting a tongue defect other than when there is concern about sealing a through-and-through communication to the neck, or a marginal mandibulectomy defect. The skin is sutured to the margins of the defect with absorbable sutures, the ends of which are left a few centimetres long. A bolster of antiseptic-impregnated gauze is placed over the skin graft and tied down with the long sutures. The bolster is removed after about 5 days.
Buccinator myomucosal flap: (Figures 27) This is an excellent flap for partial glossectomy and FOM defects as it has the same physical qualities as tissues of the FOM and oral tongue, has a reasonable amount of bulk, and preserves mobility of the tongue. Because the pedicle crosses the mandible it is particularly well suited for edentulous patients, patients with missing teeth, or who have undergone marginal mandibulectomy. (See chapter: Buccinator myomucosal flap)

Radial free forearm flap: This is a popular choice for the oral tongue as it is thin and pliable and preserves mobility of the tongue (Figure 28). An osseocutaneous flap can be used as an onlay graft for marginal mandibulectomy defects (Figure 29). (See chapter: Radial free forearm flap)
Anterolateral free thigh flap: (Figure 30) Muscle harvested with the flap can be tailored to conform to the volume of the defect to be filled. However it is less pliable than the radial free forearm flap and is only suitable for oral reconstruction in patients with thin thighs.
Free fibula flap: This is the workhorse of mandible reconstruction following segmental mandibulectomy, but can also be used as an onlay flap. It is suitable for dental implants. (See chapter: Free Fibula flap)
Pectoralis major flap: This is only used if other flaps listed are not available as it lacks pliability and provides suboptimal functional results. (See chapter: Pectoralis major flap)


Resecting tumours of the tongue is challenging particularly in terms of maintaining oral function. One should not compromise resection margins for function. The surgical team has to master an array of reconstructive techniques so as to secure the best functional outcomes.
Johan Fagan MBChB, FCORL, MMed
Professor and Chairman
Division of Otolaryngology
University of Cape Town
Cape Town
South Africa
johannes.fagan@uct.ac.za