Total glossectomy has significant morbidity in terms of intelligible speech, mastication, swallowing, and in some cases, aspiration. Consequently many centers treat advanced tongue cancer with chemo-radiation therapy and reserve surgery for treatment failures. Total glossectomy is however a very good primary treatment for carefully selected patients, especially in centers that do not offer chemoradiation. Key surgical decisions relate to whether the patient will cope with a measure of aspiration, and whether laryngectomy is required.
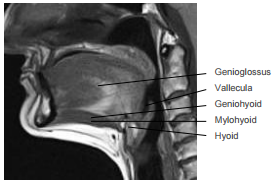
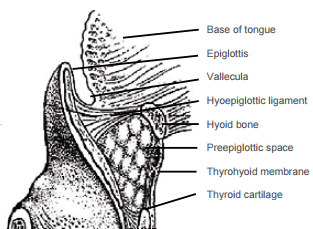
The tongue merges anteriorly and laterally with the floor of mouth (FOM), a horseshoe-shaped area that is confined peripherally by the inner aspect (lingual surface) of the mandible. Posterolaterally the tonsillolingual sulcus separates the tongue from the tonsil fossa. Posteriorly the vallecula separates the base of tongue from the lingual surface of the epiglottis.
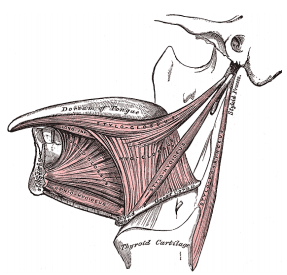
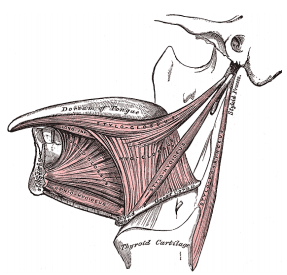
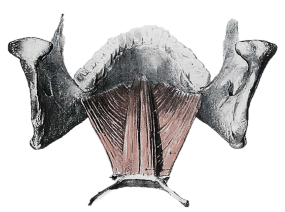
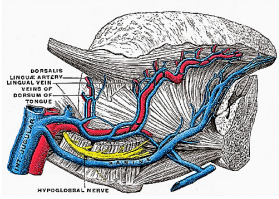
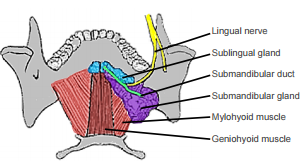
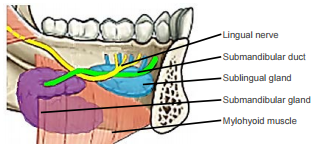
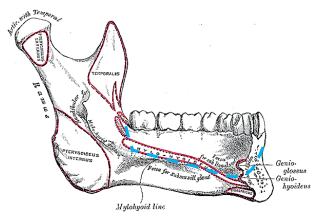
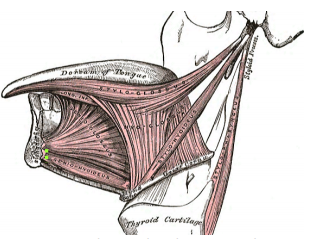
The tongue comprises eight muscles. Four extrinsic muscles (genioglossus, hyoglossus, styloglossus, palatoglossus) control the position of the tongue and are attached to bone (Figures 1, 2); four intrinsic muscles modulate the shape of the tongue, and are not attached to bone. Below the tongue are the geniohyoid and the mylohoid muscles; the mylohyoid muscle serves as the diaphragm of the mouth and separates the tongue and FOM from the submental and submandibular triangles of the neck (Figures 1, 2, 3).
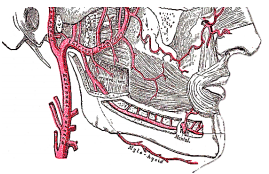
The tongue is a very vascular organ. The arterial supply is derived from the paired lingual arteries and their branches (ranine artery, dorsalis linguae, and sublingual arteries) (Figures 4, 5); and the mylohyoid artery and the submental branch of the facial artery. Additional blood supply to the tongue emanates from the tonsillar branch of the facial artery and the ascending pharyngeal artery.
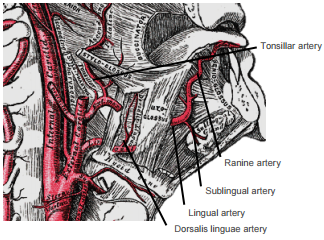
The lingual artery originates from the external carotid between the superior thyroid and facial arteries and courses obliquely forwards and medial to the greater cornu of the hyoid (Figures 4, 5). It then loops downward and anteriorly and passes medial to hypoglossal nerve (XIIn) and the stylohyoid muscle. It then courses directly anteriorly and deep to the hyoglossus and finally ascends submucosally on the undersurface of the tongue as far as its tip as the ranine artery (profunda linguae); it lies to either side of the genioglossus, and is accompanied by the lingual nerve. Two or three small dorsales linguæ arteries arise beneath the hyoglossus and ascend to the posterior part of the dorsum of the tongue and also supply the mucous membrane of the posterior FOM, and oropharynx (Figure 4). The sublingual artery branches from the lingual artery at the anterior edge of the hyoglossus and runs forward between the genioglossus and mylohyoid and supplies the sublingual salivary gland and mucous membrane of the FOM and gingiva (Figure 5). A branch of the sublingual artery pierces the mylohyoid muscle and anastomoses with the submental branch of the facial artery in Level 1b of the neck. The submental branch of the facial artery courses along the inferior, inner margin of the mandible (Figures 6).
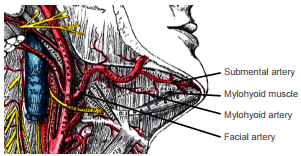
The mylohyoid artery and vein are encountered when the surgeon elevates the submandibular gland from the lateral surface of the mylohyoid (Figure 7). It branches off the inferior alveolar artery just before it enters the mandibular foramen, crosses the mylohyoid, and disappears anteriorly behind the digastric. It has connections with the submental artery and via a defect in the mylohyoid with the sublingual artery in the FOM.
Venous drainage is via lingual and ranine veins. The lingual veins originate on the dorsum, sides, and undersurface of the tongue and accompany the lingual artery and joins the internal jugular vein. The ranine veins originate below the tip of the tongue and are visible on its ventral surface; they accompany the XIIn as venae comitantes and either join the lingual vein or pass lateral to hyoglossus to join the common facial vein (Figure 4).
The following structures are located between the mucosa and the mylohyoid muscle: paired geniohyoid muscles in the midline (Figure 3); sublingual salivary glands (Figure 8, 9), submandibular ducts (Figures 8, 9), oral component of submandibular salivary glands (Figures 8, 9), and the lingual and XIIns. The paired sublingual salivary glands are located beneath the mucosa of the anterior floor of mouth, anterior to the submandibular ducts and above the mylohyoid and geniohyoid muscles. The submandibular duct is located immediately deep to the mucosa of the anterior and lateral FOM, and opens into the oral cavity to either side of the frenulum (Figures 8, 9).
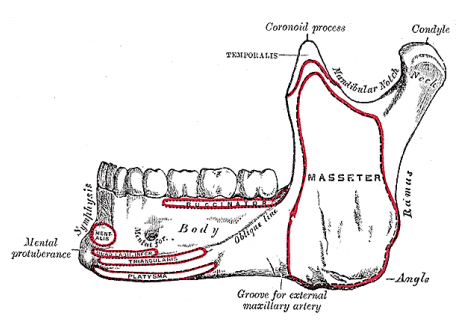
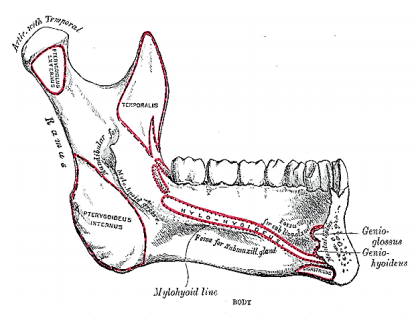
The mandible borders the FOM, and may be involved by tumour and may have to be divided for access (mandibulotomy) or resected (alveolectomy / marginal mandibulectomy / segmental mandibulectomy / hemimandibulectomy). Important surgical features are the position of the mental foramina through which the mental nerves exit to innervate the lower lip; the mylohyoid line to which the mylohyoid muscle attaches, the attachment of the genioglossus, and when planning a marginal mandibulectomy, the height of the body of the mandible and the depth of the dental roots (Figures 10a, b). In older, edentulous patients the mental foramen and inferior alveolar nerve may be very close to the superior surface of a resorbed mandible. A marginal mandibulectomy may also not be possible in such a resorbed mandible due to the lack of residual bone.
The surgeon should always stand by during induction of anaesthesia as bulky tumours may preclude elevation of the tongue to visualise the larynx and it may be difficult or impossible to intubate the patient. Should the anaesthetist be unable to intubate the larynx, the surgeon may be able to intubate through a laryngoscope, or do an emergency tracheostomy or cricothyroidotomy. Nasal intubation facilitates resection of tongue tumours, and may be followed by tracheostomy during the course of the operation. The author employs nasogastric as opposed to PEG feeding. Perioperative antibiotics are prescribed for 24hrs.
Panendoscopy is done to exclude synchronous tumours of the upper aerodigestive tract. Reassess the extent of the primary cancer, especially for posterior and lateral extension, as well as reassess the neck for cervical metastases.
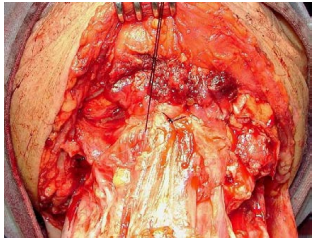
Complete the bilateral neck dissections before resecting the primary tumour (Figure 13).
Good surgical access is essential in order to attain adequate resection margins, to control bleeding, and for reconstruction. The author’s preference of a combination of transcervical and transoral access will be described. Others prefer a midline lipspit incision with mandibulotomy (See chapter: Partial glossectomy).
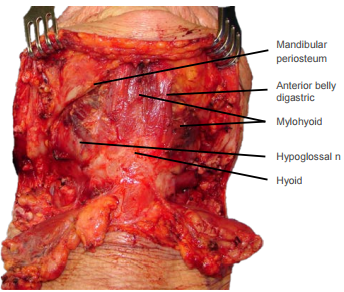
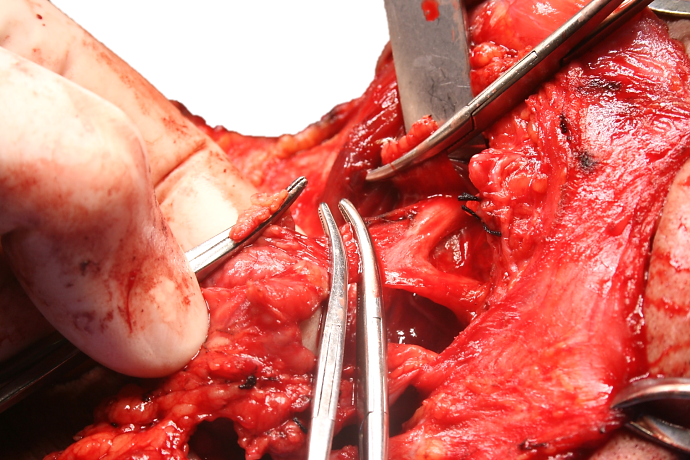
Incise the periosteum along the inferior margin of the mandible from angle-to-angle and divide the anterior bellies of digastric and the mylohyoid with electrocautery (Figure 14).
Then strip the soft tissues off the medial aspect of mandible in a subperiosteal plane. If tumour does not extend to the lateral FOM, then strip beyond the mylohyoid line to free mylohyoid from bone (Figure 15). Free the geniohyoid muscle from the inferior mental spine (Figures 15, 16)
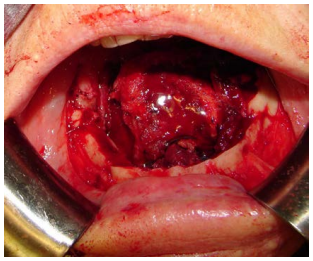
First doing a marginal mandibulectomy when tumour abuts the mandible greatly facilitates the tongue resection. Incise the gingival mucosa along the alveolar ridge (Figure 17). Strip the soft tissue off the mandible with monopolar cautery; limit exposure of the anterior surface of the mandible in order to maintain its blood supply (Figure 18). Take care (if possible) not to injure the mental nerve where it exits the mental foramen.
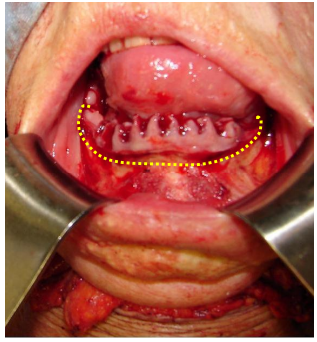
Perform a marginal mandibulectomy along the superior aspect of the horizontal ramus of the mandible as indicated in Figure 18. Angle the cut so as to include the mylohyoid line; this is especially important if tumour extends to the lateral FOM and abuts bone (Figures 15, 19). Not only does the marginal mandibulectomy have oncological relevance in terms of resection margins, but it avoids the sump effect of having a concavity along the medial border of the mandible as will become apparent later in the chapter.
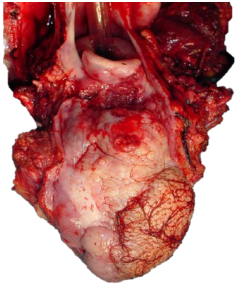
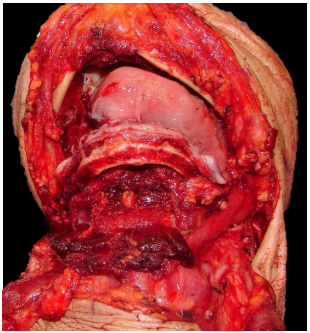
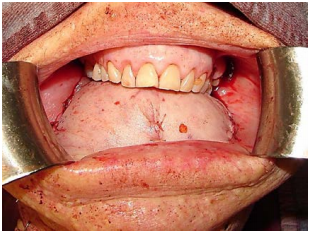
The marginal mandibulectomy, FOM and tongue are delivered into the neck (Figure 19). This permits the surgeon to resect the tongue with excellent exposure of the cancer and the vallecula (Figure 20).
Preserve as much BOT mucosa as possible to facilitate swallowing. The specimen is examined for adequacy of resection margins, and sent for frozen section if available (Figure 21).
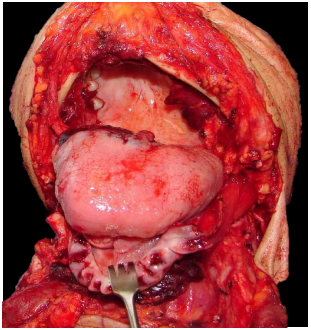
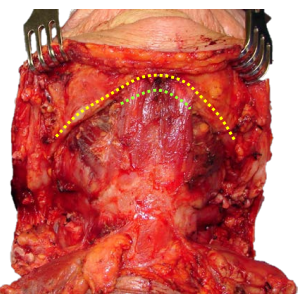
An assessment is then made about the need for total laryngectomy based on the location of the posterior margin; should the epiglottis and preepiglottic fat be uninvolved and the patient is mentally and physically fit enough to tolerate some aspiration, then one can proceed to reconstructing the defect (Figure 22).

The key functional elements of reconstruction are that the flap have enough bulk to create a convex floor of mouth so as to avoid pooling of secretions and to facilitate articulation, and that the hyoid be suspended from the mandibular arch to facilitate breathing and swallowing.
A range of flaps will provide adequate tissue volume i.e. pectoralis major (See chapter: Pectoralis major flap), latissimus dorsi, anterolateral free thigh or rectus abdominis free flaps (Figure 23). Radial free forearm flaps should not be used as they have inadequate bulk and result in a concave floor of mouth and a sump that interferes with deglutition and causes pooling and spillage of saliva and food. Mandibulectomy may necessitate free fibula flap reconstruction.
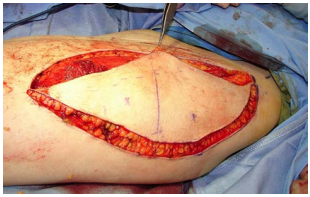
The flap should be large enough so that it bulges up to the hard palate with the knowledge that it will flatten out with time (Figures 23, 24, 25). The edges of the flap are sutured to the gingivobuccal and gingivolabial mucosae with continuous vicryl sutures (Figure 24). The aesthetic benefit of preserving the lower teeth needs to be weighed up against the fact that the teeth have limited functional value in the absence of a functioning tongue and that the lateral FOM will serve as a sump for saliva and food (Figure 26).


Laryngeal suspension is required to facilitate swallowing and to avoid obstructive sleep apnoea as all attachments of the larynx to the mandible have been severed (anterior bellies of digastric, mylohyoid, geniohyoids and genioglossus). This is achieved by suspending the hyoid bone from the anterior arch of the mandible with thick non-absorbable sutures (Figure 27).
The neck is closed over suction drains. A tracheostomy is done.
Once the patient is thought to have an adequate airway, the tracheostomy is initially corked overnight before being removed. The speech and swallowing therapist subsequently assists the patient with swallowing. Because of the absence of oral transport, this involves taking thickened liquids and pureed food initially being placed in the back of the mouth with a syringe or spoon until the patient learns to throw the head back and use gravity to assist with the oral transport phase of swallowing.
The operation is done in exactly the same manner other than the laryngectomy which is added to the procedure.
suspension is required to facilitate swallowing and to avoid obstructive sleep apnoea as all attachments of the larynx to the mandible have been severed (anterior bellies of digastric, mylohyoid, geniohyoids and genioglossus). This is achieved by suspending the hyoid bone from the anterior arch of the mandible with thick non-absorbable sutures (Figure 27).
Johan Fagan MBChB, FCORL, MMed
Professor and Chairman
Division of Otolaryngology
University of Cape Town
Cape Town
South Africa
johannes.fagan@uct.ac.za