Management of cancer of the oropharynx has undergone a paradigm shift in recent years following the realisation that HPV infection is both an aetiologic and prognostic factor for a subset of oropharyngeal squamous cell carcinoma; the introduction of transoral robotic surgery (TORS) to resect oropharyngeal tumours; as well as attempts to reduce the morbidity of chemoradiation by accepting smaller resection margins when combined with postoperative irradiation.
This chapter describes transoral and transmandibular resection of cancer of the oropharynx; it does not address the debate of the relative merits of chemoradiation vs. transoral excision using electrocautery, CO2 laser or robotics vs. open resection. Readers are referred to other chapters in the Open Access Atlas of Otolaryngology, Head & Neck Operative Surgery for detailed descriptions of Transoral laser microsurgery (TLM) and TORS, as well as for Resection of cancers of the base of tongue.
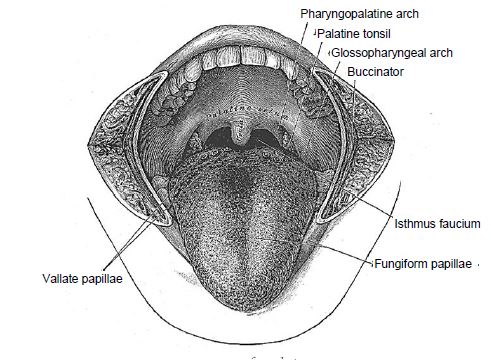
The oropharynx is comprised of the base of the tongue, tonsils, soft palate, and the lateral and posterior walls of the pharynx between the levels of the hard palate and hyoid bone.
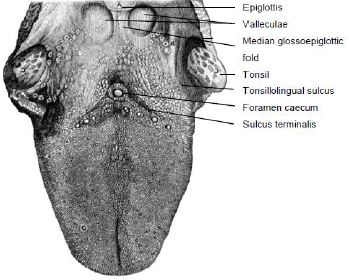
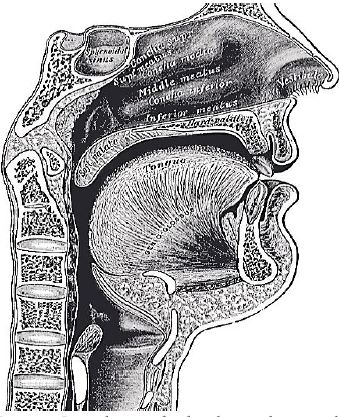
This comprises the posterior 1/3 of the tongue behind the foramen caecum and sulcus terminalis (Figure 1). The mucosa is rough, thick and fixed to the underlying muscle and contains lymphoid follicles (lingual tonsil); this makes it difficult to identify the edges of a BOT tumour; hence frozen section is especially useful to assess resection margins. Posterolaterally the tonsillolingual sulci separate the tongue from the tonsillar fossae. The valleculae separate the BOT from the lingual surface of the epiglottis and are separated in the midline by the median glossoepiglottic fold (Figure 1).
The soft palate has a complex muscular structure and innervation. It has key functions relating to speech and swallowing.
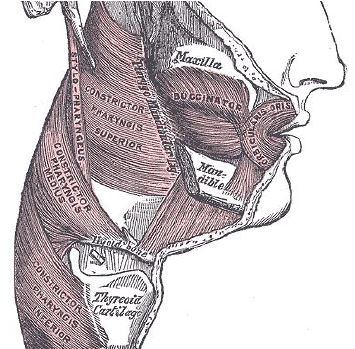
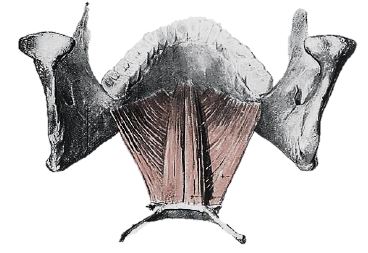
Resection and inadequate reconstruction of the palate results in loss of nasal separation which manifests clinically as nasal regurgitation of fluids and food, and hypernasal speech which can be quite disabling. The complex muscular anatomy of the soft palate and lateral pharyngeal wall is illustrated in Figure 4.

Muscles that contribute to the soft palate and lateral pharyngeal wall are summarised in Table 1.

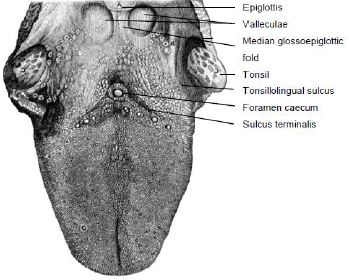
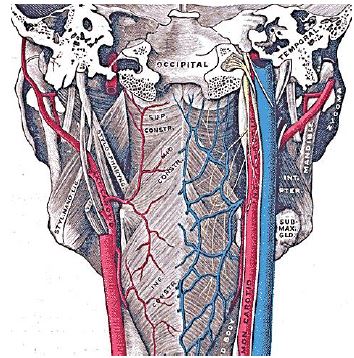
The pharynx has a number of layers i.e. mucosa, submucosa, muscle and serosa. The submucosa is represented by the pharyngobasilar fascia; it thins as it extends inferiorly from its attachment to the skull base and lines the inner aspect of the constrictor muscles. It fills the gaps between the skull base and the superior constrictor, the superior and middle constrictors, and the middle and inferior constrictors (Figure 5). Posteriorly it forms a median raphe to which the pharyngeal constrictors attach (Figure 5). The anterior faucial/tonsillar pillars are formed by the palatoglossus muscles with a thin mucosal covering and constitute the anterior limit of the oropharynx, behind which it is encircled by the superior and middle constricttor muscles (Figures 2, 4, 5, 6). The palatopharyngeus muscles constitute the posterior faucial/tonsillar pillars. The tonsils are situated between the anterior and posterior pillars, with the pharyngeal constrictor muscle lateral to the tonsil. The buccopharyngeal fascia constitutes the serosal layer; it is the outermost coat of the pharynx and is a thin layer of connective tissue that forms the anterior wall of the prevertebral space.
The only notable nerves encountered at surgery are the lingual, inferior alveolar and mental nerves, and possibly the XIIn if resection includes the lateral tongue.
The lingual nerve is a branch of V3 and provides sensory innervation to the floor of the mouth (FOM). The nerve crosses deep to the submandibular duct in the lateral FOM; in the anterior FOM it is located posterior to the duct (Figures 7, 8). It is worthwhile attempting to preserve the nerve when resecting smaller tumours in the tonsillar region.
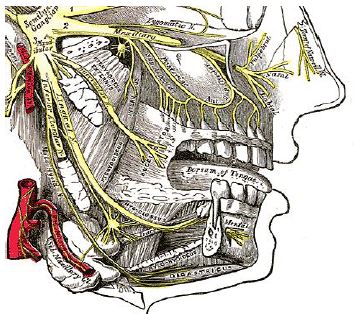
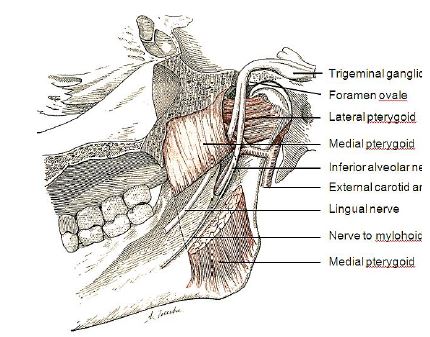
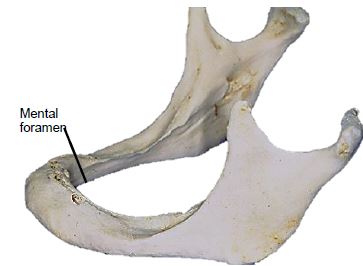
The inferior alveolar nerve and its accompanying vessels enter the mandibular canal at the lingula, and innervate the inferior alveolus and teeth (Figures 7, 8). The nerve is transected whenever a segmental mandibulectomy is done. The mental branch of the nerve exits the mandibular canal at the mental foramen to innervate the skin of the lower lip and should be preserved when doing a mandibulotomy by placing the osteotomy anterior to the mental foramen (Figure 7).
Arteries
Knowledge of vascular anatomy enables the surgeon to anticipate where arteries will be encountered and helps to minimise blood loss. Depending on the surgical procedure, vessels that may be encountered include the inferior labial, facial, lingual, inferior alveolar, mental, palatal and tonsillar arteries and the pterygoid venous plexus.
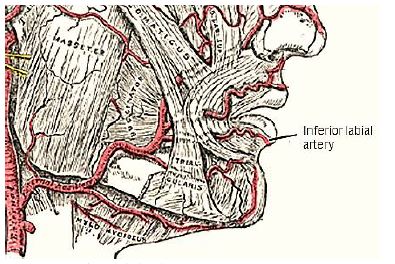
The inferior labial artery is transected when the lower lip is divided in the midline. A branch of the facial artery, it is located superficially, just deep to the surface of the lip, and is controlled with bipolar cautery (Figure 9).
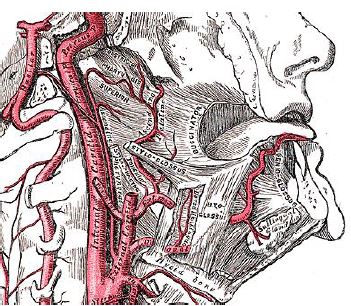
The facial artery is generally not a problem as it is reflected laterally in the cervicofacial flap that is raised when exposing the lateral surface of the mandible (Figure 9). It is commonly used as a donor vessel for free microvascular transfer flap reconstruction. The tonsillar and ascending palatine arteries are branches of the facial artery (Figure 10). The lingual artery is only encountered when resection includes the posterolateral tongue (Figure 10).
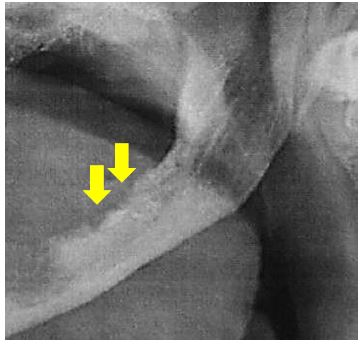
The inferior alveolar artery is a branch of the internal maxillary artery, and courses between the medial pterygoid muscle and mandible where it enters the mandibular canal at the lingula accompanied by the inferior alveolar nerve and vein (Figures 5, 8, 11).
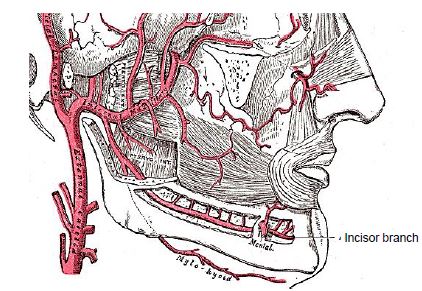
The mental artery accompanies the mental nerve and exits the mandible at the mental foramen (Figure 11). If a mandibulotomy is to be done for access just anterior to the mental foramen, avoid dissecting right up to the foramen so as not to cause bleeding requiring cautery, as this might injure the nerve. The arterial supply to the soft palate is derived mainly from the ascending pharyngeal artery, which anastomoses with the greater palatine artery at the junction of the hard and soft palate; additional supply is derived from the ascending palatine and tonsillar arteries (Figure 10). Despite transecting the soft palate with diathermy, one may encounter troublesome bleeding which is controlled with diathermy.
Muscles
The muscles of the soft palate, the pharyngeal constrictors and the palatopharyngeus and palatoglossus are generally not individually dissected and identified, but are simply resected with the primary tumour using electrocautery and scissors. Muscles that are encountered depending on the surgical approach and that are individually identified include orbicularis oris, masseter, temporalis, mylohyoid, and the medial and lateral pterygoids.
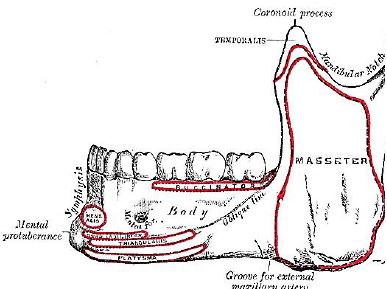
The orbicularis oris is transected with a lipsplit incision and has to be carefully reapproximated at conclusion of surgery (Figure 12). Dissecting along the lateral surface of the mandible, one next encounters the masseter muscle (Figure 12). It is a thick quadrilateral muscle with superficial and deep portions, the fibers of which converge at the insertion to the lateral aspect of the vertical ramus of the mandible (Figure 13). Both the superficial and deep portions arise from the zygoma. Laterally the muscle is covered by the parotid gland. It is innervated by V3.
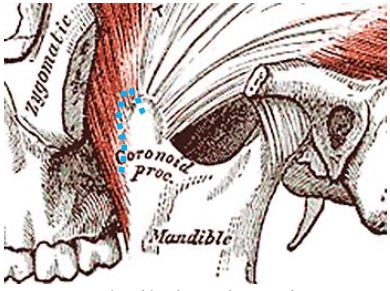
The next muscle one encounters as one dissects along the lateral surface towards the coronoid process of the mandible is the temporalis muscle (Figures 13, 14).
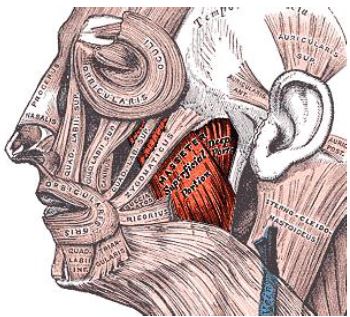
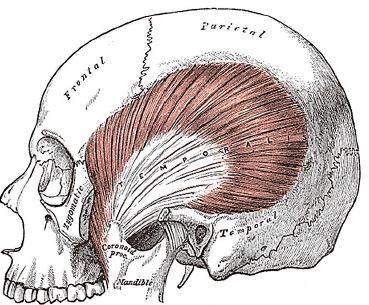
The temporalis muscle arises from the temporal fossa and temporalis fascia, and passes behind the zygomatic arch to insert onto the coronoid process and anteromedial surface of the vertical ramus (Figures 13, 14). It is innervated by V3. It receives its blood supply from the deep temporal arteries; preserving these arteries is crucial if a temporalis muscle flap is to be used to reconstruct a surgical defect.
The mylohyoid muscle is the “diaphragm” of the mouth, and is transected along the medial margin of the mandible when doing a mandibular swing approach to the oropharynx (Figures 15, 16).
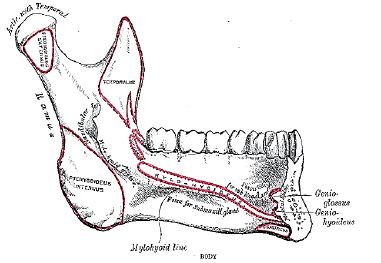
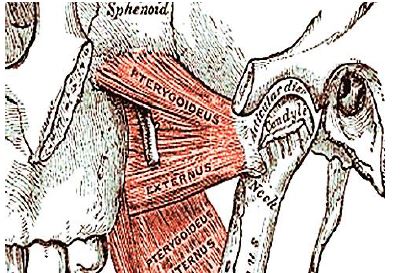
The next muscle encountered along the medial aspect of the mandible is the medial pterygoid (Figures 8, 17). It has two heads (Figure 17): the larger deep head arises from just above the medial surface of the lateral pterygoid plate; the smaller superficial head arises from the maxillary tuberosity and the pyramidal process of the palatine bone (Figure 17). The muscle passes inferolaterally to insert onto the inferomedial surface of the ramus and angle of the mandible (Figures 16, 17). It is innervated by V3.
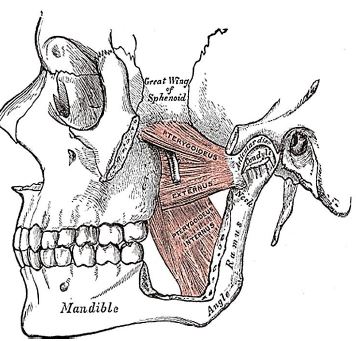
The final muscle that may be encountered is the lateral pterygoid; its superior head originates from the infratemporal surface and crest of the greater wing of the sphenoid, and the inferior head from the lateral surface of the lateral pterygoid plate (Figure 17). It inserts onto the neck of mandibular condyle and the articular disc and capsule of the temporomandibular joint (Figures 16, 17). It is innervated by V3.
The mandible may need to be divided (mandibulotomy) to gain access to the oropharynx, or the angle and vertical ramus of the mandible may be included in the tumour resection (marginal, segmental or hemimandibulectomy). Important surgical features are the position of the mental foramen through which the mental nerve exits to innervate the lower lip, the mylohyoid line to which the mylohyoid muscle attaches, and when planning a marginal mandibulectomy, the height of the body of the mandible and the depth of the dental roots (Figures 13, 16). The mental foramen and inferior alveolar nerve may be very close to the superior surface of a resorbed mandible such as is seen in older, edentulous patients (Figure 18). A marginal mandibulectomy may not be possible in such a resorbed mandible due to the lack of residual bone.
The remainder of this chapter focuses on the surgical treatment of the primary tumour.
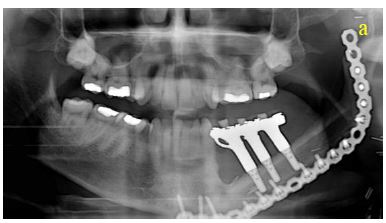
Invasion of cortical bone is better assessed with CT; MRI is superior for assessing medullary invasion. In the absence of CT scans the surgeon may elect to strip tumour off bone at the time of resection taking care not to seed tumour, inspect the bone for evidence of periosteal and bony infiltration, and then decide how to proceed. If only the periosteum is involved then a marginal mandibulectomy (removal of cortical bone) may suffice. Should marginal mandibulectomy be considered, then the vertical height of the mandible should be assessed clinically or by Panorex so as to predict whether a free bony composite flap would be required to strengthen the remaining mandible. Once the cortex is invaded, then either marginal or segmental mandibulectomy is required. Medullary invasion requires segmental or hemimandibulectomy that includes at least a 2cm length of mandible on either side of the tumour
The surgeon always stands by the patient’s side during induction of anaesthesia as it may be difficult or impossible to intubate a patient who has a bulky tumour, or who has trismus. Should the anaesthetist be unable to intubate the larynx, the surgeon may be able to intubate through a laryngoscope, or do an emergency tracheostomy or cricothyroidotomy; it is prudent to inject the tracheostomy or cricothyroidotomy site with local anaesthetic (with adrenaline) prior to induction. Nasal intubation facilitates resection of pharyngeal tumours, and is converted to a tracheostomy during the course of the operation.
Good surgical access is essential in order to attain adequate resection margins, to control bleeding, and for reconstruction. A combination of surgical approaches can be used, and will now be discussed. Level 1 of the neck should first be dissected before proceeding to address the primary tumour if neck dissection is indicated.
Transoral resection with electrocautery (Bovie)
Transoral access varies considerably. Edentulous patients are generally better suited to transoral resection. A useful way to predict whether transoral resection is likely to be possible is to pull on the anterior tongue with a cotton swab during preoperative clinical evaluation and to then see how accessible the tumour is. Note that tumours becomes more visible and accessible as the resection proceeds, especially once the thick BOT lining has been incised around tumour.
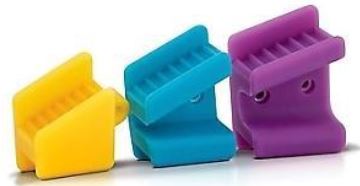
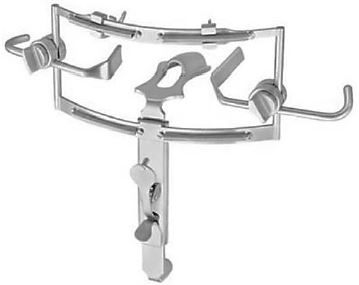
The mouth is kept wide open either with a dental bite block (Figure 20), or with a self-retaining retractor, taking care to protect the teeth from injury (Figure 21), or with a tonsil gag or Dingman retractor (Figure 22).
Perioperative antibiotics are prescribed for 24hrs.

Apply traction to the tongue and the tumour with silk traction sutures or with tissue forceps (Figure 21). Resect the tumour with at least a 1cm margin of normal tissue using electrocautery (Bovie). As the resection proceeds, insert new silk traction sutures or reapply the tissue forceps to facilitate delivery of the tumour.
Mandibulotomy with mandibular swing
This affords excellent access to the oropharynx. It does however leave a facial scar; it may cause deformity of the lower lip; there is a risk of complications relating to the mandibulotomy and dental malocclusion; and the lingual nerve is at risk of injury.
Having completed the Level 1 neck dissection, the vermillion border is scored or marked so as to ensure an accurate repair (Figures 23, 24).

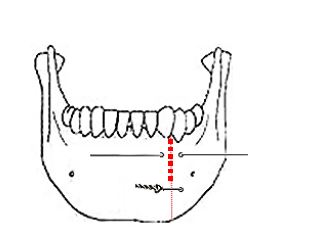
The lower lip is vertically divided in the midline (Figure 25). Bleeding from the inferior labial artery is controlled with bipolar cautery. At this point, some surgeons prefer to do a median mandibulotomy; it is however the authors’ preference to do a paramedian mandibulotomy.

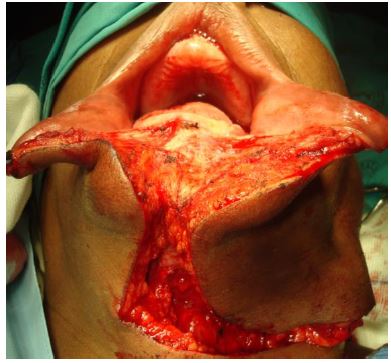
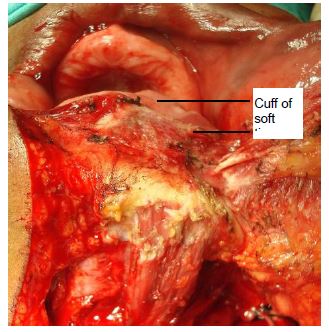
Incise the gingivolabial and gingivobuccal mucosae >0.5cms from the bone so as to leave a cuff of soft tissue on the bone to facilitate subsequent soft tissue closure (Figure 26). Strip soft tissue off the mandible with monopolar cautery or with a periosteal elevator stopping just short of the mental foramen so as not to injure the mental nerve or mental artery where it exits the foramen (Figure 26).
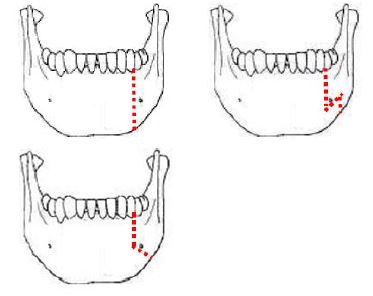
A paramedian mandibulotomy is done just anterior to the mental foramen. Compared to median mandibulotomy, the advantages are that it is closer to tumour, it does not disturb the genioglossus, geniohyoid, and digastric muscles, there is less disruption of the FOM, and should segmental mandibulectomy be required, then only the lateral mandible is sacrificed. The mandible is divided just anterior to the mental foramen with a Gigli or a powered saw (Figure 27). The osteotomy may be made vertically or alternatively in a step- or V-shaped fashion so as to achieve a more stable repair (Figure 28). It is advisable to extract a tooth and make the osteotomy through the dental socket to avoid devitalising adjacent teeth.

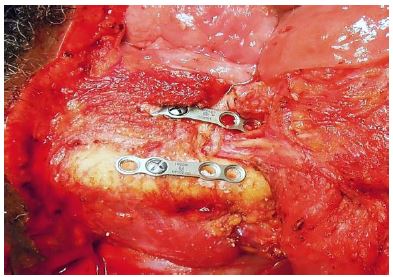
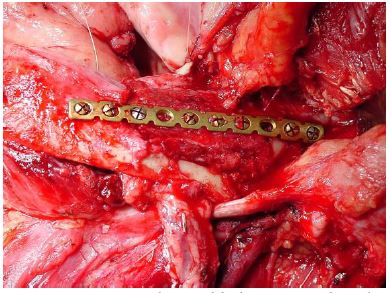
In dentate patients the mandible is preplated with titanium miniplates contoured to the mandible to ensure perfect dental alignment. Two 4-holed, non-compression, 2mm mandibular plates, one placed along the inferior border of the mandible and the other placed more superiorly, are used (Figure 29). Once the plates have been contoured and the holes drilled, they are removed and the bone cut is made.
The surgeon then distracts the cut ends of the mandible to gain access to the oral cavity and proceeds to divide the FOM mucosa and mylohyoid muscle about 1cm from, and parallel to, the mandible, so as to leave soft tissue on the mandible for FOM repair at conclusion of the surgery. Continue the incision posteriorly along the FOM until the tumour comes into view; the lingual artery (medial to the hyoglossus muscle) and the XIIn course medial to the FOM incision and are not at risk of injury at this stage of the dissection.
The tumour is resected using electrocautery. Posteriorly the lingual nerve extends from the skull base, passes behind medial pterygoid and crosses the incision line from lateral to medial to course along the lateral FOM; preserve the nerve if possible.
At the conclusion of surgery the FOM is closed with a running vicryl suture, and the osteotomy is plated; when plating sets are not available, opposing holes are drilled on either side of the osteotomy and the mandible is wired together with stainless steel wires (Figure 31).
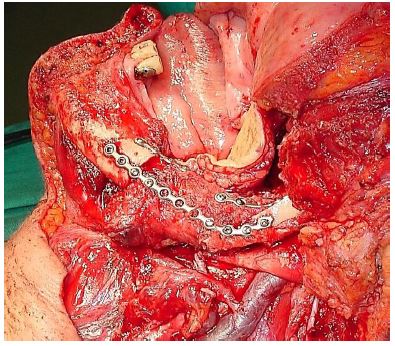
Marginal mandibulectomy is done for access, for securing adequate oncologic resection margins, or to facilitate mucosal repair by suturing gingivolabial to gingivobuccal mucosa (Figure 32). Segmental mandibulectomy is done to secure adequate oncologic margins (Figure 33).
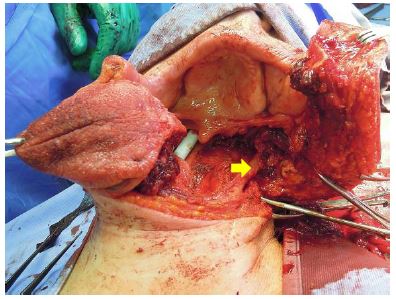
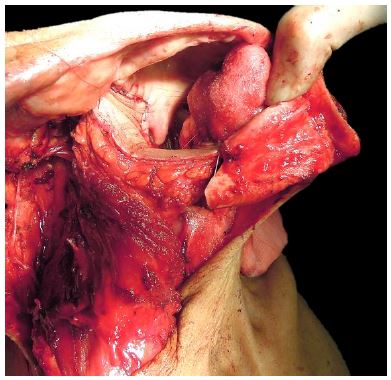
The initial surgical steps are as described for paramedian mandibulotomy (up to Figure 26). Transect the mental nerve and artery with cautery, and continue to strip soft tissue off the lateral aspect of the mandible up to the masseter muscle; then strip the masseter off its mandibular insertion using electrocautery (Figures 34, 35).

Inspect the tumour, and make a decision as to whether marginal, segmental or hemimandibulectomy is required to obtain clear margins and then plan the osteotomies. Use an oscillating/reciprocating saw or a Gigli saw for the osteotomies (Figure 36). Beware of the close proximity of the external carotid artery and its branches to the vertical ramus when making the osteotomies (Figures 5, 11).
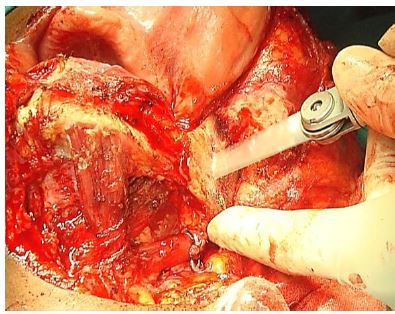
With a segmental mandibulectomy in a dentate patient one should preplate the mandible with a reconstruction plate to ensure an accurate repair and perfect dental occlusion.
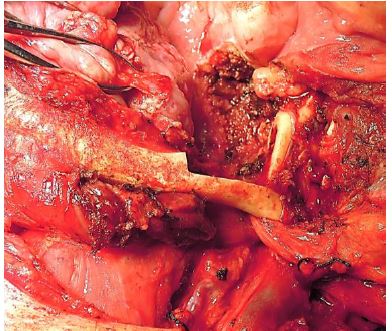
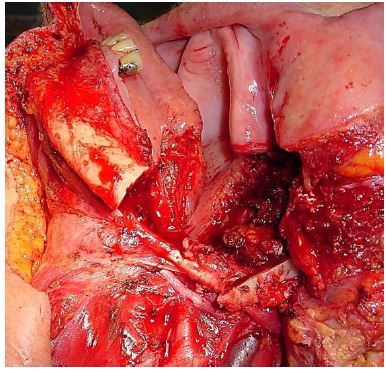
To resect the coronoid process, strip the masseter off the entire length of the vertical ramus, identify the mandibular notch, and while pulling caudad on the mandible, free the insertion of the temporalis muscle from the coronoid with cautery, keeping close to bone throughout to avoid blood vessels situated medially; this step is simpler if the distal osteotomy has already been done (Figure 37).
It is generally not necessary to resect the condyle; rather carefully transect the condylar neck bearing in mind the proximity of the internal carotid artery. To resect the condyle, transect the lateral pterygoid at its insertion onto the condylar neck and the joint capsule (Figure 38).
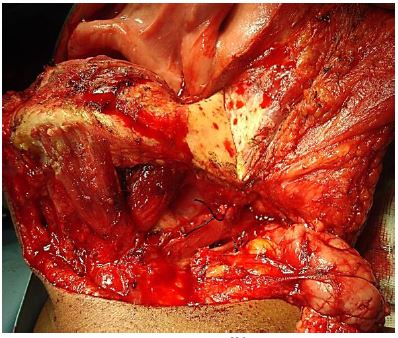
Tumour resection
With adequate exposure, resecting the tumour is generally quite straightforward using electrocautery (Figures 39 a, b). The surgeon has to remain aware of the locations of the internal and external carotid arteries; palpating the styloid process is useful as the internal carotid artery lies medial to the bone.
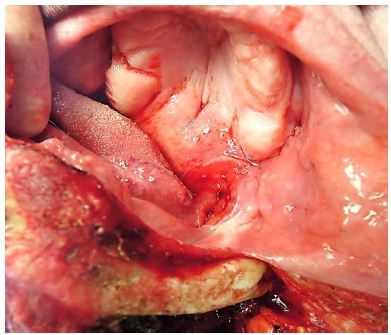

Orientate the tumour for the pathologist with a silk suture (Figure 39b); obtain frozen section of the margins if available.
Obtain meticulous haemostasis using ties, monopolar and bipolar cautery before closing the defect.
The lip is carefully repaired in layers to approximate the muscles as well as mucosa and skin.
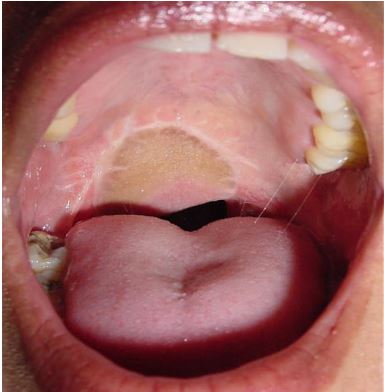
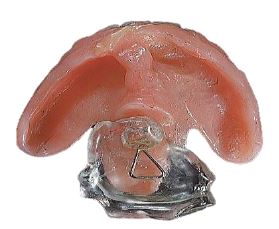
The pharynx is a complex functional unit. Whether and how to repair or reconstruct oropharyngeal defects requires that a surgeon critically follows his/her patients and learns from successes and failures. Poor repairs and reconstructions cause hypernasal speech and nasal regurgitation. Failure to reconstruct a lateral mandibular segmental defect (allowing mandible to “swing”) may have significant cosmetic and functional consequences (Figure 40).
Healing by secondary intention is not utilised frequently enough with BOT resections, but is of course commonly employed with tonsillectomy, TLM and TORS.

Primary closure of BOT defects yields the best swallowing results, although inadequate bulk impairs speech if the BOT cannot approximate the soft palate. Primary closure of palatal defects may cause hypernasal speech and nasal regurgitation.
Pedicled and free tissue transfer flaps may be used to reconstruct oropharyngeal defects. Simply shaping a flap to match the resected tissue may well restore form yet have a poor functional result. Therefore one has to carefully assess the defect to determine how best to optimise function.
Buccinator myomucosal flap: (See chapter: Buccinator myomucosal flap) A posteriorly-based buccinator flap can be used to repair defects of the soft palate, lateral pharyngeal wall and BOT. It is an excellent choice as it has the same physical qualities as tissues of the oropharynx, has a reasonable amount of bulk, and preserves mobility (Figure 41).
Pectoralis major flap: (See chapter: Pectoralis major flap) Although this is a reasonable option to use, it may drag down on the soft palate causing palatal incompetence. It is a useful soft tissue filler of a lateral segmental mandibular defect (Figure 42).

Buccal fat pad flap: (See chapter: Buccal fat pad flap) This is a useful flap to cover exposed mandible or maxillary bone, or to augment a thinned out soft palate, or to close a small soft palate defect.
Temporalis muscle flap: (See chapter: Temporalis muscle flap) This is commonly used in some centers for oropharyngeal defects. The muscle is pedicled on the coronoid process which is immediately adjacent to the oropharynx. It requires that the deep temporal arteries be preserved.
Radial free forearm flap (RFFF): This is a thin, pliable flap and is therefore an excellent option for oropharyngeal repair (Figures 43-45). It can also be used as an onlay osseocutaneous flap following marginal mandibulectomy.

Anterolateral free thigh flap: Muscle harvested with the flap can be tailored to conform to the volume of the defect to be filled. However it is less pliable than the radial free forearm flap and is therefore less suited to soft palate reconstruction.
Free fibula flap (FFF): (See chapter: Vascularised free fibula flap). This is the workhorse flap for patients requiring reconstruction of mandible (Figure 46).

Final comments
Resecting tumours of the oropharynx is challenging particularly in terms of access and optimising swallowing and speech. One should not compromise resection margins for function. The surgical team has to master an array of surgical approaches and reconstructive techniques to ensure the best oncological and functional outcomes.
Johan Fagan MBChB, FCORL, MMed
Professor and Chairman
Division of Otolaryngology
University of Cape Town
Cape Town
South Africa
johannes.fagan@uct.ac.za
Eugene N Myers MD, FACS, FRCS Edin (Hon)
Distinguished Professor & Emeritus Chair
Department of Otolaryngology
Eye and Ear Institute, Suite 519
200 Lothrop Street
Pittsburgh, PA 15213
USA
myersen@upmc.edu