Sialoliths vary in size, shape, texture, and consistency; they may be solitary or multiple. Obstructive sialadenitis with or without sialolithiasis represents the main inflammatory disorder of the major salivary glands. Approximately 80% of sialolithiasis involves the submandibular glands, 20% occurs in the parotid gland, and less than 1% is found in the sublingual gland. Patients typically present with painful swelling of the gland at meal times when obstruction caused by the calculus becomes most acute. When conservative management with sialogogues, massage, heat, fluids and antibiotics fails, then sialolithiasis needs to be surgically treated by transoral, sialendoscopic and sialendoscopy assisted techniques; or as a last resort, excision of the affected gland (sialadenectomy).
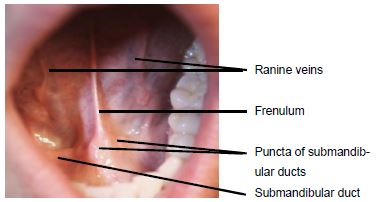
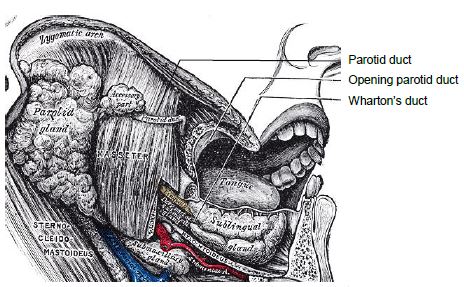
The paired submandibular ducts (Wharton’s ducts) are immediately deep to the mucosa of the anterior and lateral floor of mouth (FOM) and open into the oral cavity to either side of the frenulum (Figure 1). The frenulum is a mucosal fold that extends along the midline between the openings of the submandibular ducts.
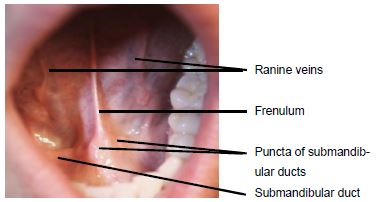
The anterior FOM has a covering of delicate oral mucosa through which the thin-walled sublingual/ranine veins are visible (Figures 1 & 2). The veins are visible on the ventral surface of the tongue, and accompany the hypoglossal nerve (Figure 2).
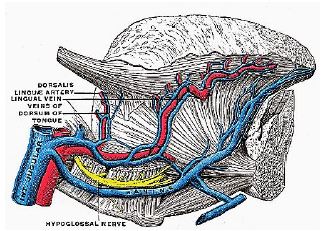
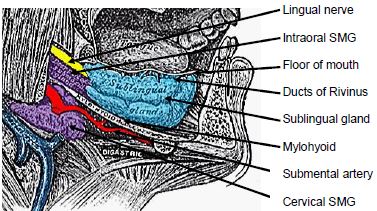
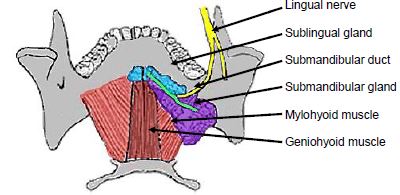
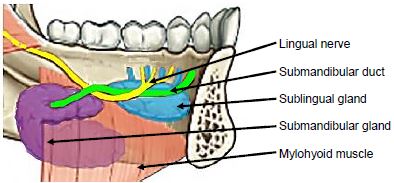
The paired sublingual salivary glands are located beneath the mucosa of the anterior FOM, anterior to the submandibular ducts and above the mylohyoid and geniohyoid muscles (Figures 3 & 4). The glands drain via 8-20 excretory ducts of Rivinus into the submandibular duct and also directly into the mouth on an elevated crest of mucous membrane called the plica fimbriata which is formed by the gland and is located to either side of the frenulum of the tongue).
In the anterior floor of mouth the lingual nerve is located posterior to the duct; it crosses deep to the submandibular duct in the lateral floor of mouth (Figures 3, 4, 5).
The parotid (Stensen’s) duct exits the anterior edge of the parotid gland, and crosses the surface and hooks around the anterior aspect of the masseter, traverses the buccal fat pad, and pierces the buccinator muscle to enter the mouth opposite the 2nd upper molar (Figure 6).
Visual scanning of submandibular, preauricular, and postauricular regions is the first step to assess for the presence of swelling and erythema; this is followed by intraoral examination. The salivary ductal orifice may be red and oedematous. One should massage the gland to milk and inspect the saliva; frank infection may be represented by plaques or whitish secretions emanating from the duct. Manual palpation of the parotid gland allows a surgeon to determine the consistency of the gland.
Bimanual palpation (finger inside and outside the mouth) is particularly important when examining the submandibular gland and its duct.
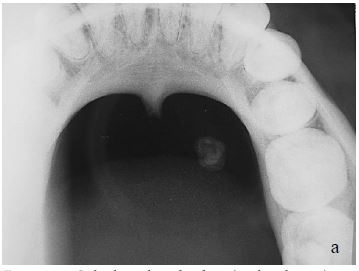
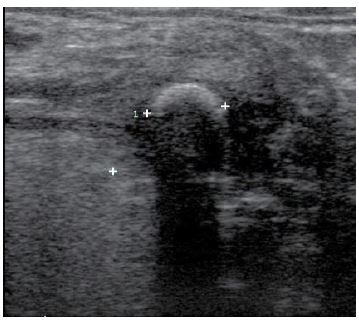
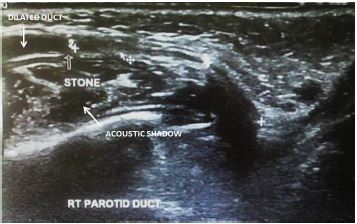
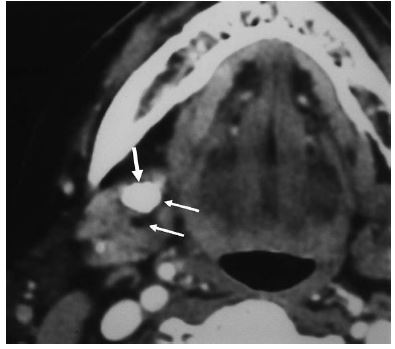
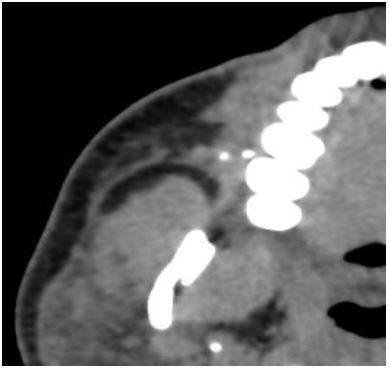
Imaging modalities for inflammatory conditions of glands are plain X-rays (Figures 7a, b), sialography (Figure 8), ultrasound (Figure 9), and computed tomography (Figure 10).
Plain X-rays have less value with parotid stones because of the higher percentage (60-70%) of radiolucent stones; approximately 20% of submandibular stones are not visible with plain X-rays.
Sialography provides images of the morphology of the ductal system and allows diagnosis of strictures, dilatations, and filling defects (Figure 8).
MR sialography is good means to measure ductal stenosis. Although avoiding ionising radiation, it has less resolution than conventional sialography, thereby limiting visualisation of the peripheral ducts.


Ultrasound (Figure 9) is noninvasive and has no associated discomfort. Failure to detect a stone with ultrasound is not uncommon as the distal portion of the submandibular and parotid ducts can be difficult to visualise using extraoral ultrasound; and ultrasound may be of limited value for the deep portion of the submandibular gland. An obstructed duct that may otherwise not be evident may be better visualized after giving the patient something sour like lemon juice or sour sweets as this may cause ductal dilatation with obstructive pathology (Figure 10).
Computed tomography (CT) imaging is a good imaging modality to see sialoliths (Figures 11, 12). Another advantage is its ability to diagnose and locate intraparenchymal stones and calcification.
Limitations of ultrasound and CT include distinguishing non-echogenic stones from strictures, determining the length of a stenosis and the diameter of the duct distal to an obstruction. Ultrasound is a dynamic and operator-dependent investigation and pathology may be therefore be overlooked.
Prior to sialendoscopy, sialoliths in the submandibular duct and gland were divided into two groups:
Note: Although feasible in selected cases, the same sialolithotomy procedure for the more posterior ductal region carries a significant risk of injury to the lingual nerve and the possibility of severe bleeding from the lingual vessels (Figure 2).
Prior to the advent of sialendoscopy, sialoliths in the parotid duct and gland were divided into two groups:
The 1st step therefore is to precisely locate the stone to select a surgical approach.
Traditional Intraoral Parotid Sialolithotomy
Suture the ductal layer to the oral mucosa with several 4/0 Vicryl sutures to maintain ductal patency
The difference between parotidectomy for sialolithiasis and a benign tumour is the condition of the gland; inflammation, scarring and fibrosis both inside the gland and around Stensen’s duct make the operation difficult and heighten the risk of facial nerve injury.
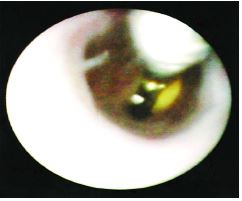
Salivary gland endoscopy has been a major advance, not only in terms of providing an accurate means of diagnosing and locating intraductal obstruction, but for permitting minimally invasive surgery that can successfully relieve blockages not amenable to intraoral approaches. Sialendoscopy also permits both diagnostic assessment and definitive treatment in the same operative session. 1
Acute sialadenitis is a contraindication as the risks of ductal injury and perforation are increased due to the inflammation and inability to visualize during the procedure from purulent material within the duct.
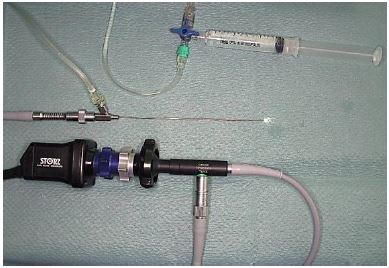
Rigid and semi-rigid endoscopes have a larger diameter, greater stability, and can be autoclaved (Figures 15, 16). Instrumentation includes an array of grasping forceps, balloons, baskets, graspers, burrs, lasers fibers, and stents (Figure 17).



Introducing the endoscope into the ductal papilla, the narrowest portion of the duct, can be challenging. The following methods progressively lead to accomplishing this:



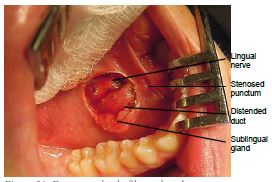
Stenosis of the papilla of Wharton’s duct may require a cut-down procedure onto the duct; dissecting the sublingual gland laterally and exposing the duct and lingual nerve deep to the duct; and then inserting the sialendoscope. Healing is by secondary intention, or ductoplasty (suturing edges of the duct to the floor of mouth at the end of the procedure) can be performed. With this approach, the duct is best opened along its length superiorly, with the size of the cut limited to the size of the scope used, firstly to avoid transecting the duct and secondly to facilitate not diminishing the hydrostatic pressure required to dilate the duct during the procedure due to escape of wash around the scope.
Saline irrigation is used to expand the otherwise collapsing duct distally. The saline is delivered from a 50-100mL syringe via intravenous tubing which is attached to the irrigation port of the endoscope (Figure 16).
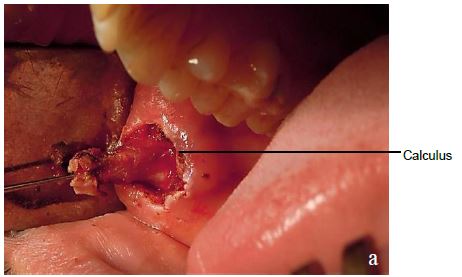
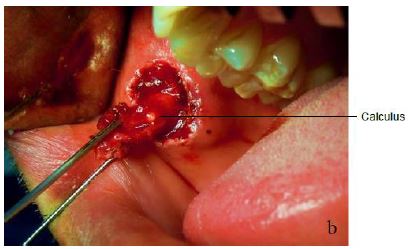
Stones located distally (<1cm) from the punctum of Wharton’s duct can be removed by slitting the duct along its length with insulated needle-tip electrocautery, removal of the lith/stone, followed by sialendoscopy and lavage of the ductal system. The duct heals by secondary intention, and stents are not required to prevent stenosis.
Figure 21 illustrates the unusual situation of a duct that is completely fibrosed at the punctum following removal of a distally located calculus; the distended duct has been exposed (note lingual nerve immediately behind the duct). In Figure 22 the duct has been transected and translocated to the lateral floor of mouth; absorbable sutures anchor the walls of the duct to the oral mucosa.

Alternatively, treatment for distal stones <5 mm is by interventional sialendoscopy. Papillotomy frequently has to be performed to deliver the calculus because the ostium is the narrowest part of the duct.
Mobile stones located proximally within Wharton’s duct and measuring <5mm, are best removed by interventional sialendoscopy using baskets passed through the working channel of the sialendoscope (Figures 17c, 23).

Once a stone is engaged in the basket it often cannot be released. Therefore the basket is passed beyond the stone and only then opened so as to avoid the risk of entrapping an immobile, large stone. Another technique is to hold and extract the stone with grasping forceps, without bypassing the stone (Figures 17g, 24).
Larger stones may be fragmented with a hand drill (Figure 17e) and with forceps (Figures 17g, h)); this can be time consuming. Calculi measuring >5mm and located in the proximal part of Wharton’s duct can be removed by Nahlieli et al.’s ductal stretching procedure 2 (Figure 25) and by limited duct incision.
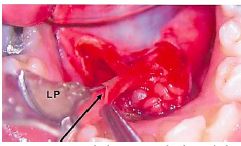
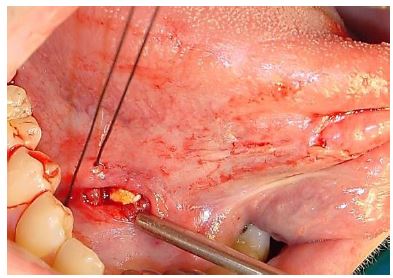
A safe surgical approach requires a detailed knowledge of the ductal and lingual nerve anatomy, good exposure with a mouth prop, and lateral retraction of the sublingual gland with stay sutures passed between the teeth. 3
Repairing the duct proximally can be technically challenging; leaving it open usually has a good outcome. Incising the duct from punctum to hilum and then suturing the duct to the floor of the mouth usually avoids ductal stenosis 4. Alternatively Marchall 5 stents the duct. A guide wire is passed through the working channel of the sialendoscope and through a ductotomy; the sialendoscope is withdrawn; a stent is advanced over the guide wire; the stent is sutured to the papilla with a nonabsorbable suture and is left in situ for about 3 weeks.
Proximal submandibular stones >5mm in diameter and not able to be removed by transoral techniques can be treated with Extracorporeal Shock Wave Lithotripsy (ESWL) followed by sialendoscopy. Because of the high calcium content of submandibular calculi, this technique is less successful compared to parotid calculi that have lower calcium content. ESWL is not available or approved for calculi in many countries including the USA.
Dissecting along the parotid duct from its oral end may cause stenosis. Interventional sialendoscopy and basket retrieval is the treatment of choice of both proximal and distal parotid stones measuring <4-5mm. Small calculi not amenable to intervenetional sialendoscopy, and stones measuring >5mm can be treated with ESWL (if available) followed by sialendoscopy. If ESWL is not available, sialendoscopy with any of the various intracorporial fragmentation techniques described above may be performed. Alternatively, a gland-sparing approach using an external parotid approach combined with sialendoscopy is advocated for calculi of >5mm within Stensen’s duct. Stones are located endoscopically or by intraoperative ultrasound if there is a stenosis distal to the stone. Coloured silastic tubing passed up the duct helps to stabilise the duct. An external parotid approach is then used to locate the stone. Nerve monitoring is used, because the duct crosses several branches of the facial nerve. Stensen’s duct is then slit length-wise and the stone is removed. The duct is repaired using 7-0 Prolene. Stenoses can be repaired with a vein graft ductoplasty patch. Check that the closure is watertight by means of transoral back-pressure saline irrigation of Stensen’s duct administered via the irrigation channel of the sialendoscope. Fibrin glue may help to secure a salivary seal. Sialostenting introduced either externally or via a sialendoscope and advanced over a guide wire is recommended for 2-4 weeks.
With both submandibular and parotid stones, ESWL followed by sialendoscopy can be performed. A better outcome can be expected for parotid stones (lower calcium content). Multiple intraparenchymal symptomatic stones not amenable to conservative therapy are treated with sialoadenectomy. Where ESWL is not available, sialoadenectomy is advocated for fixed intra-parenchymal stones and stones not amenable to the gland-sparing techniques. An expertly performed sialoadenectomy carries a low risk of complication to cranial nerves (V, VII, and XII) and it is a once-off event for the patient without a concern for xerostomia. A balanced informed consent should include sialoadenectomy as an alternative initial approach.
A variety of lasers have been used for intracorporeal lithotripsy, among them the XeCl excimer, flash-lamp pulsed dye, the Ho:YAG, and the erbium:YAG laser. An important advantage of most lasers is that the fibers are of small diameter, sometimes only 200µm, yet allow one to deliver high-watt intensities to fragment stones even in the peripheral the ductal system or behind stenotic segments. Visibility is often compromised by floating fragments which are removed by irrigation, baskets, or forceps before proceeding. Lasers used for intracorporeal lithotripsy are expensive, time consuming, carry a risk of perforating the duct, may require multiple procedures, and can result in the development of abscesses requiring gland removal.
The severity of complications is generally quite modest and includes ductal perforation, basket entrapment, ductal avulsion, postoperative infection and ductal strictures, swelling in the floor of mouth with potential airway compromise and recurrence of symptoms. 6 Risks associated with transoral submandibular approaches include lingual nerve injury and bleeding. Transfacial sialendoscopic approaches can result in trauma to the buccal branches of the facial nerve and formation of a sialocoele; this is managed with Botox (Allergan, Inc. Irvine, CA) and anticholinergics, but is best avoided by a creating a watertight seal and using tissue glue.
Success is measured by treatment that is efficient, clinically effective, cost effective, and gland sparing. Diagnostic and interventional sialendoscopy, and sialendoscopy-assisted and transoral techniques have been a major advance, not only by providing an accurate means of diagnosing and locating obstruction, but also permitting minimally invasive surgical management that can successfully address sialolithiasis, and preclude sialoadenectomy in most cases.
Multiple or combined measures may prove effective. A flexible methodology is still required. 7
Robert L Witt MD, FACS
Professor of Otolaryngology-Head & Neck Surgery
Thomas, Jefferson University
Philadelphia, PA, USA
RobertLWitt@gmail.com
Oskar Edkins MBChB, MMed, FCORL
Otorhinolaryngologist
Division of Otolaryngology
University of Cape Town
Cape Town, South Africa
o.edkins@uct.ac.za