Management of small tumours involving the true vocal folds can be contentious. Tumour control is achieved in over 95% of patients presenting with T1 glottic cancer employing external beam radiation thera-py, vertical hemilaryngectomy, or transoral endoscopic resection. Given adequate re-sources, the weight of evidence favours endoscopic transoral resection as the most cost-effective approach with very high rates of tumour control.
Young patients presenting with involvement of the anterior commissure or partial impairment of motion (T2) and those who have failed attempts at curative irradiation therapy for small glottic lesions may be suitable candidates for vertical partial laryngectomy.
When the tumour requires removal of the anterior commissure, the proper term for this procedure is frontolateral partial laryngectomy. Frontolateral vertical hemilaryngectomy can be accomplished to include one arytenoid and, when necessary, both true vocal folds. Under these circumstances, some surgeons may choose supracricoid partial laryngectomy with cricohyoido-epiglottopexy to manage extensive cancer of the anterior commissure involving both vocal cords and the paraglottic space.
Vertical partial laryngectomy is not suitable for tumours involving the supraglottic larynx and the paraglottic space. Similarly, it is not appropriate for patients with greater than 10 mm of subglottic extension. Involvement of both arytenoids is also a strict contraindication.
Patients presenting with multifocal lesions, diffuse dysplasia and carcinoma in situ, involvement of the arytenoids and the posterior commissure, and those in whom poor health compromises suitability for surgery may be better served with external beam irradiation.
When considering surgical intervention for cancer involving the true vocal cords, precise staging and patient selection are crucial for good outcomes. High resolution fine-cut CT compliments microlaryngoscopy and examination under anaesthesia.
In the setting of failed prior irradiation therapy, the surgeon must be aware of the potential for multifocal persistent cancer. In general, the entire field of the original tumour should therefore be considered for removal.
Careful preoperative tumour mapping employing flexible fiberoptic endoscopy and fine cut CT allows the surgeon to estimate the extent of resection and the reconstructive needs of each individual patient. For instance, patients requiring frontolateral hemilaryngectomy in which both arytenoids are intact and 80% of one vocal cord can be maintained will require no added tissue for reconstruction.
Conversely, if an arytenoid is resected or if more than 20% of the contralateral vocal fold must be removed, some reconstruction must be undertaken to afford good swallowing without aspiration and to allow adequate diameter of the lumen for respiration.
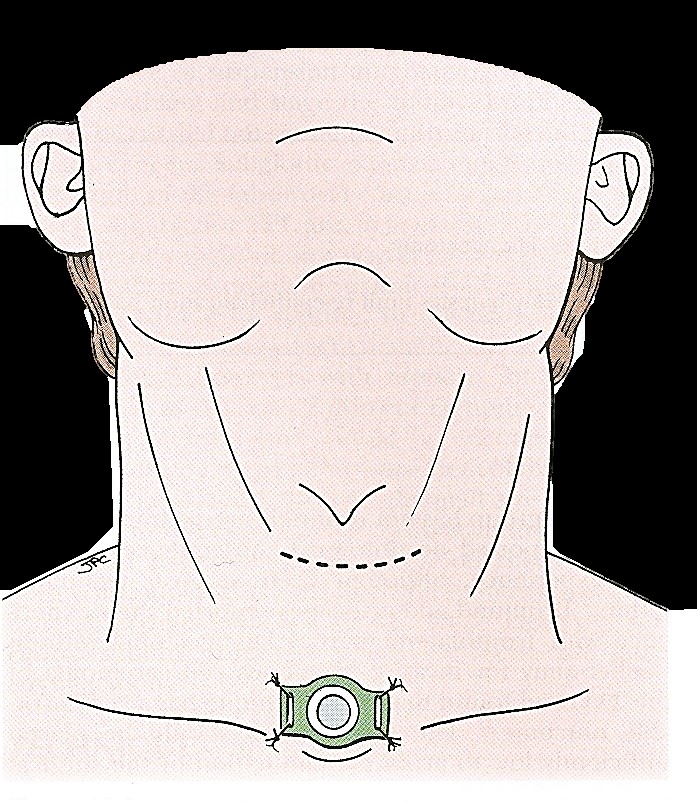
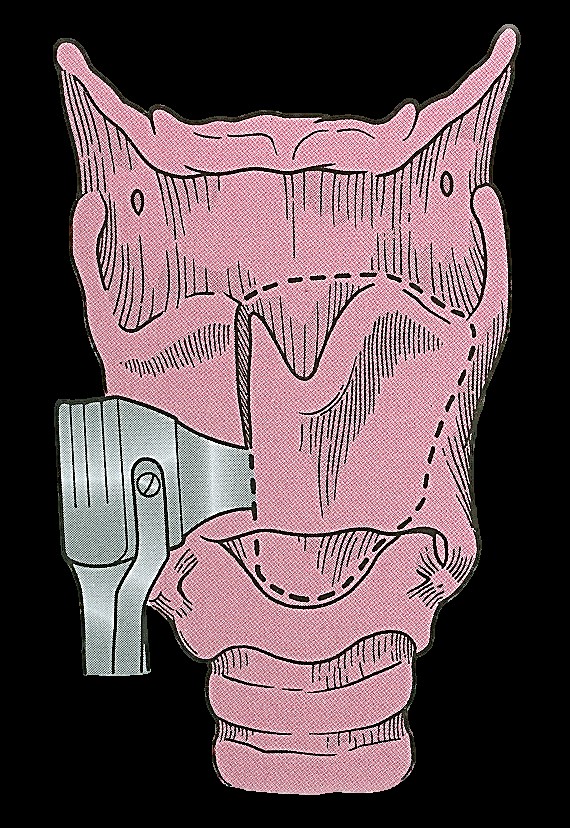
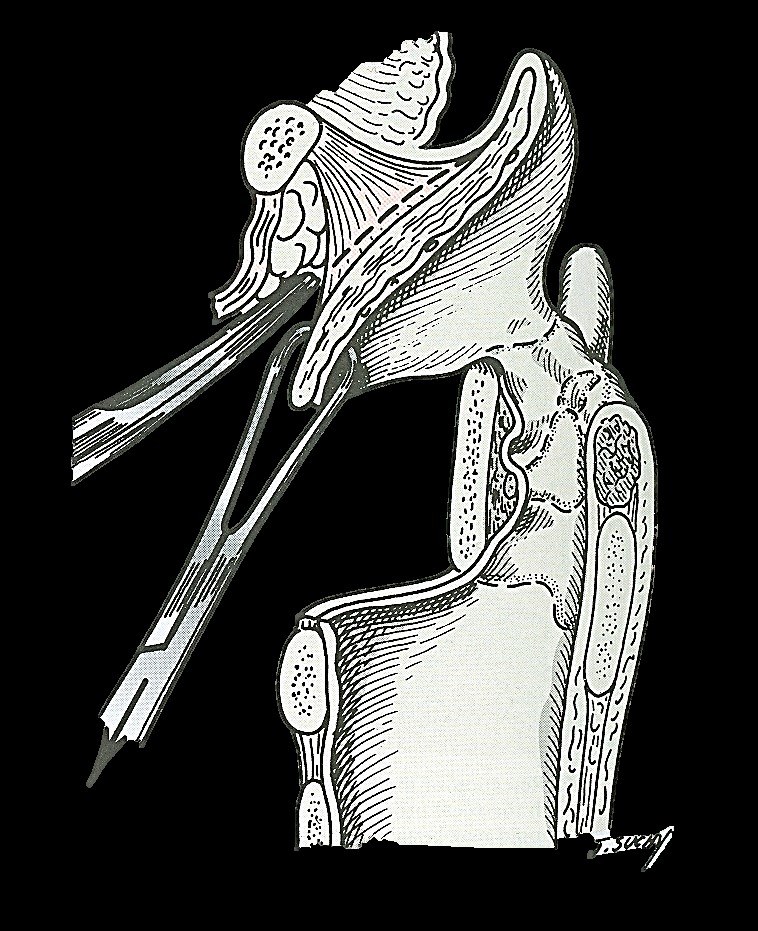
The procedure is undertaken under general anaesthesia. Perioperative prophylactic antibiotics are administered. Tracheotomy is accomplished through a separate incision. A second horizontal incision is made at approximately the level of the thyroid notch (Figure 1).
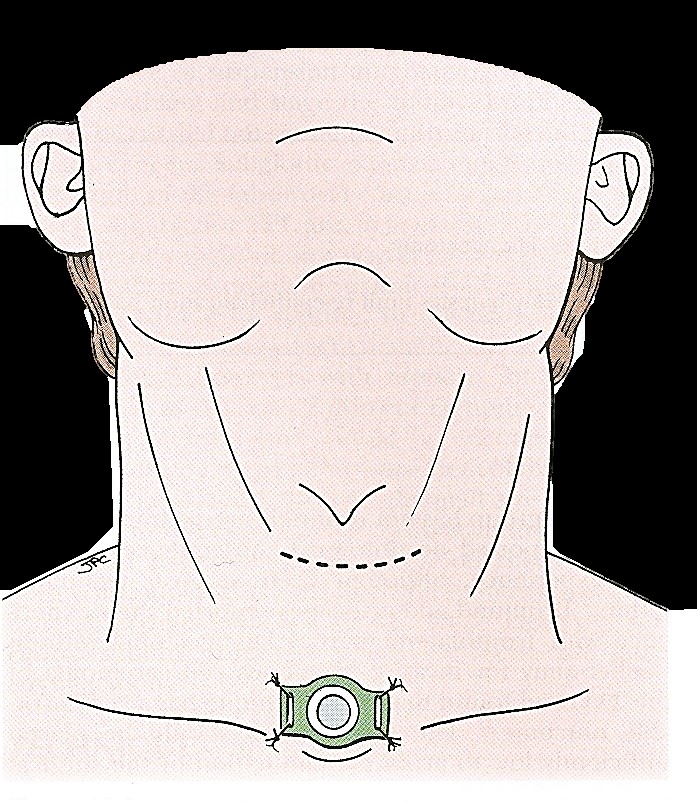
Skin flaps are elevated superiorly to the hyoid and inferiorly to the cricoid cartilage. The strap muscles are then elevated, exposing the thyroid lamina.
The external perichrondrium of the thyroid cartilage is incised at the midline and a posteriorly-based perichrondrial flap is elevated bilaterally (Figures 2 & 3).
The extent of the elevation should reflect the intended thyroid cartilage resection.
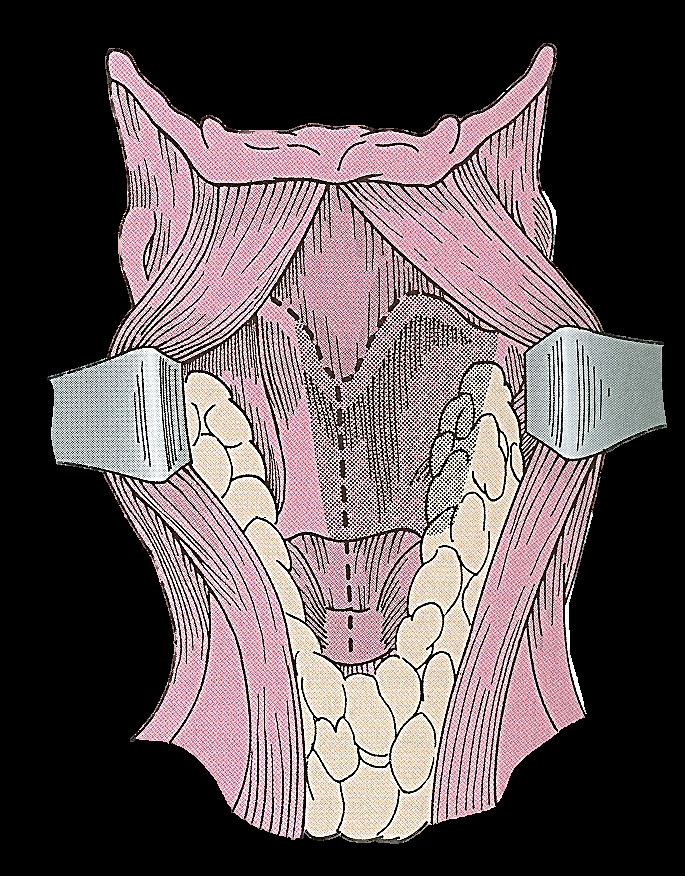
Vertical cuts are then made through the thyroid cartilage, maintaining as much of the posterior lamina of the cartilage as basic oncologic principles will allow (Figure 4).
It is essential that the cartilage cuts be made perpendicular to the plane of the cartilage and that soft tissue cuts be made with a knife (not with a saw) (Figure 5).
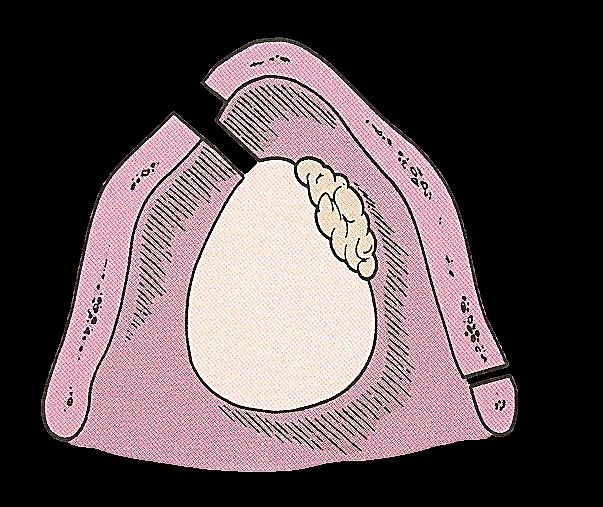
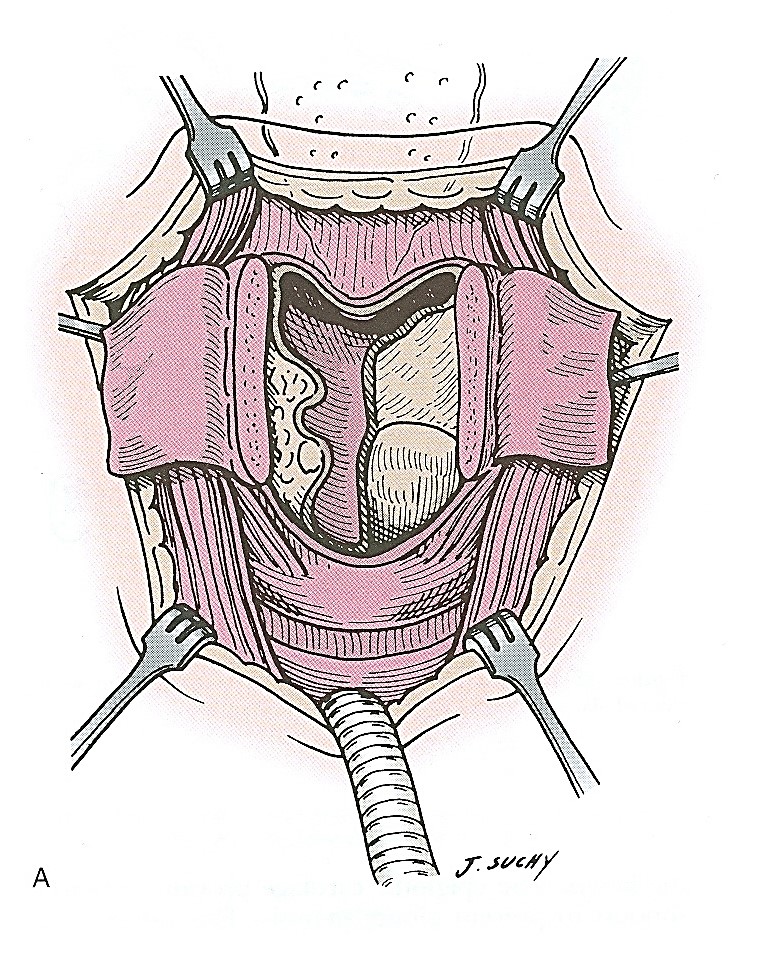
A wide cricothyrotomy allows access to the subglottis such that the surgeon working with a headlight and a knife can visualize the undersurface of the vocal cords and to place the initial cut to allow a 2 mm margin from the tumour without unnecessarily removing uninvolved vocal fold. The thyrotomy is then opened widely such that the cut across the posterior aspect of the involved vocal fold can be accomplished with a 2 mm margin and the specimen removed. New margins from both sides of the vocal cord should be submitted for frozen section assessment. A nasogastric tube is introduced and fixed to the nasal septum with a suture.
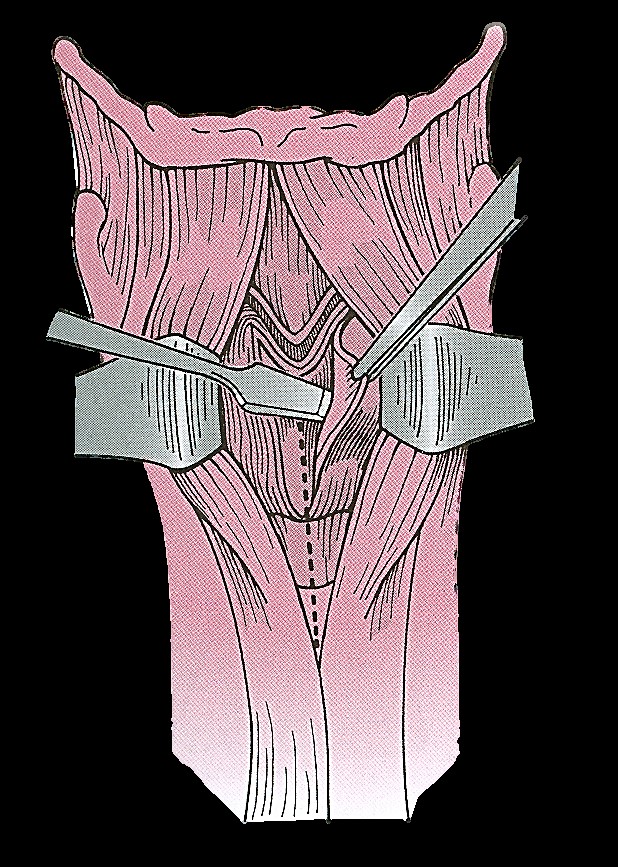
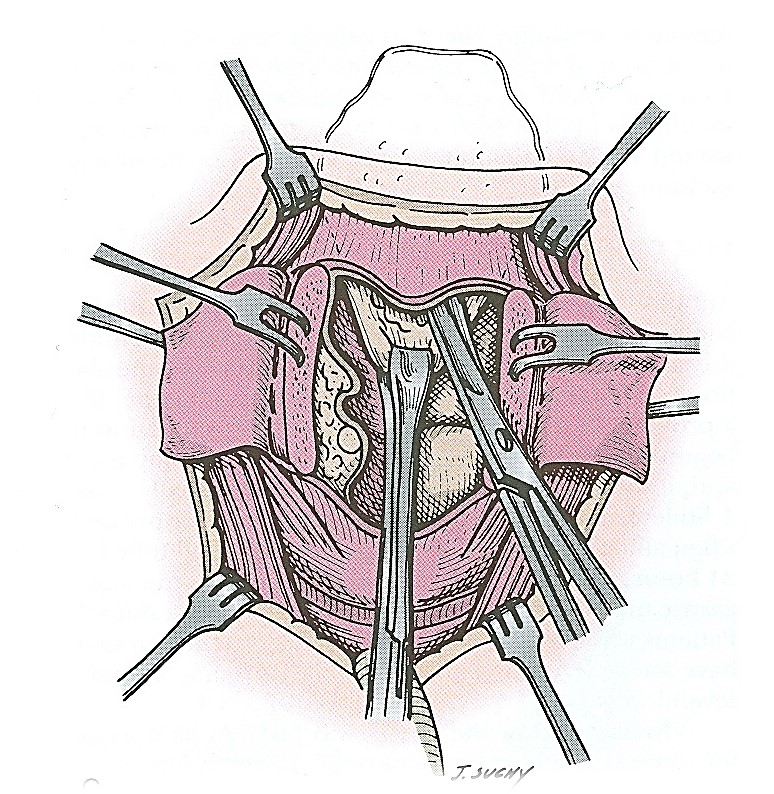
When two-thirds or more of one vocal fold has been preserved, no extra soft tissue reconstruction is required. The free end of the residual vocal fold must be fixed anteriorly to the residual thyroid cartilage with a vicryl suture (Figure 6).
Reconstruction is accomplished by closing the external perichondrium in the midline (Figure 7). The strap muscles are re-approximated in the midline as the second layer of closure.
A Penrose drain is inserted. Suction drains should be avoided because they will tend to pull secretions through the wound. The skin is reapproximated in layers and a cuffed tracheotomy tube is introduced.
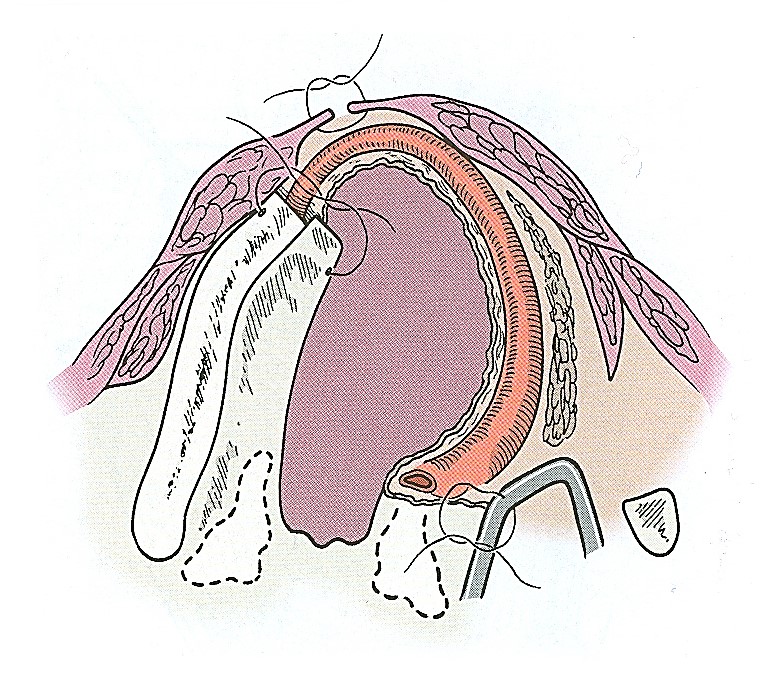
When more than 20% of the contralateral vocal fold cannot be maintained, some form of tissue reconstruction is required to reconstitute the lumen to maintain an adequate airway. I prefer employing an epiglottopexy. The petiole of the epiglottis is grasped with an Allis forceps, and the hyoepiglottic ligament freed such that the epiglottis can be mobilized and pulled inferiorly and fixed to the superior surface of the cricoid cartilage (Figures 8 & 9).
When tumour considerations require removal of the body of the arytenoid, it, too, must be reconstructed. The critical aspect is to reestablish the height of the arytenoid to prevent secretions from flowing directly from the pharynx into the larynx. A multitude of techniques have been reported employing cartilage, muscle or just fat.
The tissue needs to be fixed to the top of the cricoid and then covered by advancing mucosa from the medial wall of the pyriform sinus over the reconstructive materials. Patients requiring arytenoid reconstruction invariably have prolonged recovery and temporary dysphagia.
At completion of the procedure, the patient should have a cuffed tracheotomy tube in place with the balloon inflated. Antibiotic administration is terminated on the first postoperative morning. The patient’s nutritional needs are supported by feeding through a nasogastric tube.
The dressing supporting the Penrose drain should be changed for good hygiene. The drain can be removed when it is no longer producing mucoid secretions. Ordinarily that occurs on the third or the fourth postoperative day.
Routine tracheotomy care is provided. The tracheotomy cuff should be maintained inflated for 4-5 days to divert coughed secretions through the tracheotomy tube rather than into the newly reconstructed wound.
On the fifth postoperative day, the tracheotomy cuff can be deflated. This allows the treatment team to determine if the patient can protect his own airway without aspiration. Patients who have previously been treated with radiation therapy may have a delayed decannulation process. If the patient tolerates deflating the cuff on the tracheotomy tube, the treatment team can change the tracheotomy tube to a smaller, uncuffed tube. The adequacy of the reconstructed airway can be tested by plugging the tracheotomy tube.
Patients who tolerate this overnight are candidates for decannulation. Soft foods are reintroduced and the patient can be discharged.
Salvage following Radiation: Special Considerations and Problems
The most common call for frontolateral partial hemilaryngectomy in the era of transoral endoscopic technology is to treat patients with persistent cancer after having had radiation therapy. Such patients have increased oedema, slower healing, and a high incidence of chondritis. The drain frequently needs to be maintained beyond the first week. Antibiotic administration should be instituted for cellulitis and erythema. Return to oral eating is often delayed and the nasogastric tube may need to be maintained for 2-3 weeks. Under these circumstances, the majority of patients can be discharged to home with home nursing and care of the tracheotomy and nasogastric tube until the wound has stabilized, oedema has resolved, at which time the treatment team can proceed with the decannulation and oral feeding process.
Partial vertical hemilaryngectomy is highly effective (>90%) in properly selected patients. Surgical removal of previously irradiated tumours always has the potential that multifocal tumour is overlooked and if not completely removed, will recur.
All patients having open partial laryngectomy have dysphonia post-operatively. The overwhelming majority of patients do however have a serviceable voice.
Longstanding dysphagia and aspiration are unusual as long as both arytenoids are preserved or, when one arytenoid has been removed, it has been appropriately reconstructed.
Failure to properly reconstruct the glottis after resection of the majority of both vocal folds will result in laryngeal stenosis. Prevention is the key to relief of this problem. The treatment team must recognize the need for extra soft tissue and incorporate the reconstruction at the time of resection. Reconstructing the stenotic larynx is beyond the scope of this chapter.
Jonas T. Johnson, M.D.
The Dr Eugene N. Myers Professor and Chairman
Department of Otolaryngology
Eye and Ear Institute
200 Lothrop Street
Suite 500
Pittsburgh, PA 15213
USA
johnsonjt@upmc.edu
Johan Fagan MBChB, FCORL, MMed
Professor and Chairman
Division of Otolaryngology
University of Cape Town
Cape Town
South Africa
johannes.fagan@uct.ac.za