A high percentage of HIV-infected persons are nasal carriers of Staphylococcus aureus, hence the high rate of infection in this population.
Description: Impetigo is a superficial bacterial skin infection characterised by flaccid pustules and honey-coloured crust. It usually begins as a small painful erythematous papule.
Aetiology: The most common implicated organism is Staphylococcus aureus, although group A beta- hemolytic streptococcus (Streptococcus pyogenes) has been implicated in some cases.
Clinical presentation: Impetigo can be bullous and non-bullous, usually on the face and extremities. Primary impetigo presents as erythematous plaques with or without thin-walled vesicles that break down leaving characteristic yellow crust. Secondary impetigo can occur in other dermatoses e.g. eczema.
Epidemiology: Impetigo is common in children especially those aged 2-5 years and prevalence of 15-25% has been reported in the tropics. It is transmitted by contact with infected skin.
Diagnosis: Diagnosis is usually clinical but a Gram stain and culture may be required to confirm diagnosis when there is extensive disease.
Treatment: This should be guided by local antibiotics sensitivity testing but in mild and localized infection, first-line topical antibiotics like mupirocin, bacitracin or fusidic acid for 7-10 days are effective. If the infection is widespread, severe or is associated with lymphadenopathy, oral penicillins (flucloxacillin) or macrolides (erythromycin) if patient is allergic to penicillins, are indicated for 7-10 days. Parenteral antibiotics may be required if impetigo is diagnosed in a very sick child.
Complications: Cellulitis, osteomyelitis, staphylococcal scalded skin syndrome, and acute post- streptococcal glomerulonephritis can occur.
Prevention: Regular care of healthy skin and minimal skin contact with an infected child reduces the risk of transmission. Prompt diagnosis and treatment will prevent complications. In settings where impetigo is endemic among children, measures to reduce the transmission frequency should be adopted, including encouraging regular hand washing, educating the population on health matters and instituting treatment early in the course of the disease.


Description: Folliculitis is the inflammation of the hair follicle. It can be caused by physical injury, chemical irritation or an infection.
Aetiology: Staphylococcus aureus is the most frequent cause of infective folliculitis but folliculitis can also be caused by pathogenic fungi e.g. Candida albicans, commensal fungi such as Malassezia furfur and mites such as Demodex species. These are most often seen on the face in immunosuppressed children.
Clinical presentation: The presentation may be in the form of itchy, painless or painful papules, dome-shaped pustules (with hair shaft at the centre) often with an erythematous base. Folliculitis has predilection for the scalp, extremities, occluded areas and areas prone to excessive moisture and chafing. Systemic symptoms are not common.
Epidemiology: It is a common bacterial skin infection in childhood.
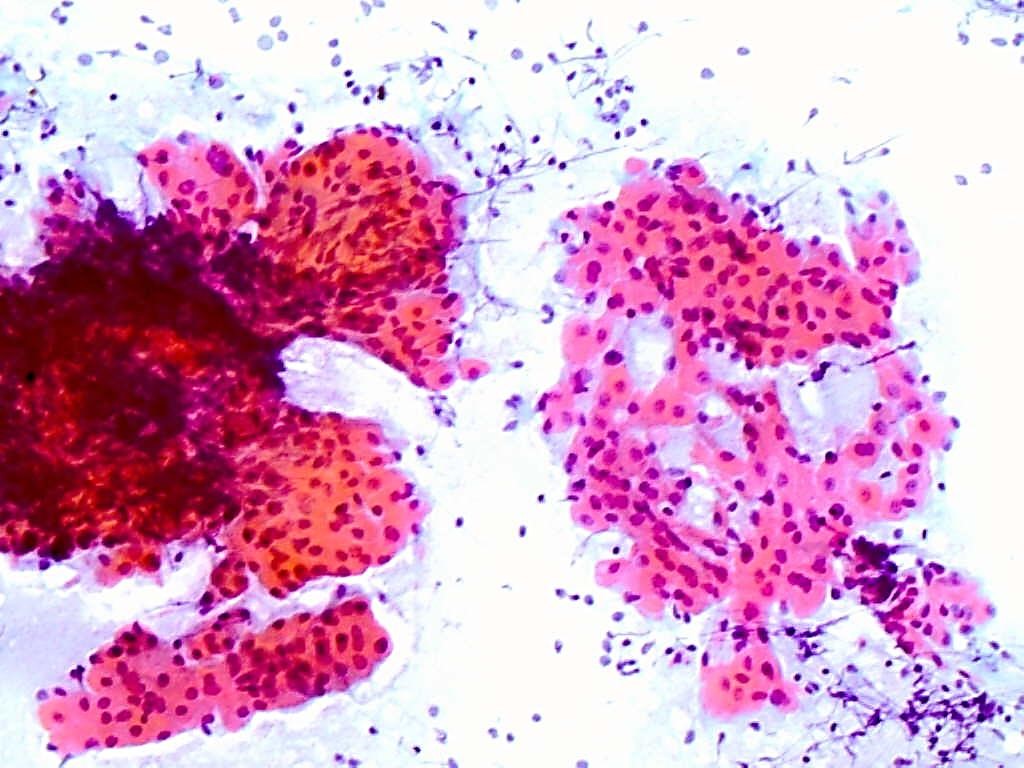
Diagnosis: It is a clinical diagnosis, but Gram stain and culture of pus may be required to confirm diagnosis.
Prevention: Prompt diagnosis and treatment reduces spread of the disease. Regular care of healthy skin reduces infection rates will prevent complications. Treatment of Staphylococcus carriers, particularly caregivers of affected children is important in reducing transmission and recurrence. Those who participate in sports should shower regularly and not share personal clothing.
Treatment: Mild staphylococcal folliculitis is often self-limiting, or may respond to cleansing or topical antiseptics. In more severe cases, antibiotics, topical or systemic, may be required. Topical mupirocin may suffice for mild infection. For deep-seated infection, oral antibiotics should include coverage for S. aureus, such as penicillinase-resistant penicillins e.g. flucloxacillin or macrolides – e.g. erythromycin. First-generation cephalosporins such as cephalexin may also be used.
If the infection is persistent or recurrent, the usual sites of staphylococcal carriage should be sought in the patient, contacts or caregivers and anti-staphylococcal measures initiated. Application of ½ strength hibitane cream or mupirocin cream to nostrils twice daily for 5 days is indicated. This has to be repeated monthly as re-colonization is common.
Complications: These include furuncles, carbuncles, septicaemia and osteomyelitis all of which may be recurrent.

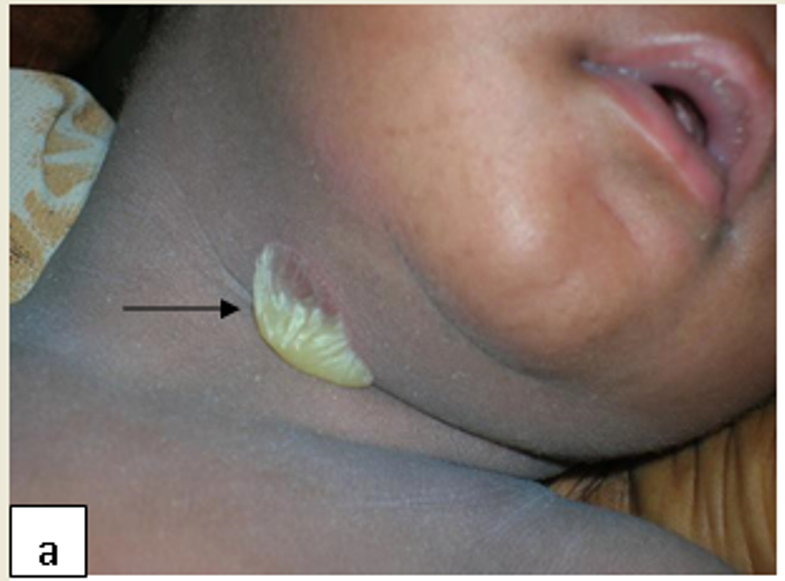
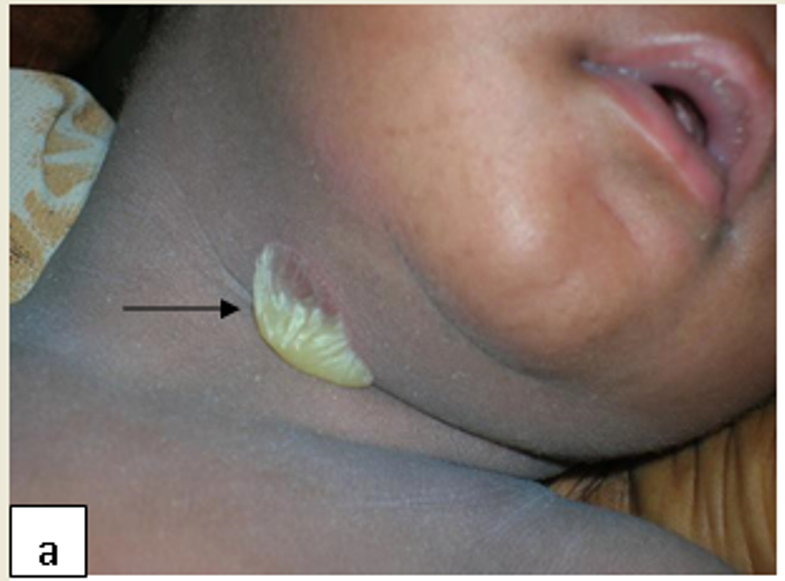
Description: Furunculosis (boil or abscess) is inflammation of the hair follicle with small abscess formation extending through the dermis into the subcutaneous layers. When furuncles aggregate to form broad, swollen, erythematous, deep, and painful masses that usually open and drain through multiple tracts they are called carbuncles.
Aetiology: Furunculosis is suppurative sequelae of a folliculitis. Staphylococcus aureus is the primary aetiological agent.
Clinical presentation: A furuncle appears as a red tender, firm, erythematous, often fluctuant nodule on hair-bearing parts of the body, with central purulence that may spontaneously drain. They are most often seen on the neck, face, buttocks, axillae, and groin.
Epidemiology: It is transmitted by contact with infected skin and other fomites. It is often spread to other family members. Predisposing factors include poor hygiene, overcrowding, immunodeficiency and malnutrition.
Diagnosis: Clinical but Gram stain and culture of pus may be required to confirm diagnosis.
Prevention: Family hygiene including regular hand washing, fomite cleaning, and avoiding contact with contaminated skin. In recurrent cases effort should be made to exclude diabetes and other causes of immunosuppression. Nasal and perineal carriage of Staphylococcus aureus in the patient and other household members should be sought and treated.
Treatment: May resolve spontaneously, but surgical drainage of pus is mainstay of therapy. If surrounding cellulitis or systemically unwell, cloxacillin IV 25 – 50 mg/Kg/dose 6 hourly or flucloxacillin PO may be indicated. Treatment of recurrent furunculosis involves therapeutic triad of antibiotics, decolonisation and decontamination.
Complications: These include carbuncles, septicaemia, osteomyelitis and scarring.




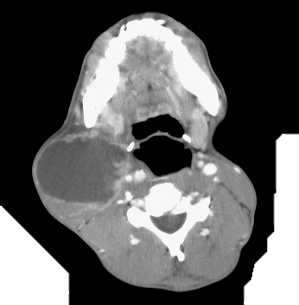
Definition: An acute bacterial infection (also known as “flesh eating bacteria”) that is characterized by necrosis of the deep fascia and subcutaneous tissues. It is a progressive and rapidly spreading infection in the deep tissue planes.
Aetiology: NF can be classified as polymicrobial (type I) or monomicrobial (type II), type I being more common. Type I NF is caused mainly by a combination of Group A Streptococcus (most common), Klebsiella, Clostridium, E. coli, Staphylococcus aureus, and Aeromonas hydrophila.
Clinical presentation: Pain, swelling and redness at the site of infection, followed by frank necrosis within days or weeks. Constitutional symptoms and signs such as fever, tachycardia and tachypnoea may be present. Presence of crepitus indicates gas produced by aerobic and anaerobic organisms is considered diagnostic of NF, but together with haemorrhagic bullae, skin necrosis, crepitus, sensory and motor deficits, it is a late sign of NF.
Epidemiology: Most common in immunocompromised hosts such as patients with HIV infection and diabetics.
Diagnosis: NF is a clinical diagnosis and Gram stain, blood and tissue cultures aid management.
Treatment: Surgical debridement, fasciotomy and broad spectrum intravenous antibiotics are the mainstay of treatment. Initial antibiotic treatment could include penicillin G and an aminoglycoside. Clindamycin may be added to cover streptococci, staphylococci, gram-negative bacilli, and anaerobes. Antibiotics are adjusted with culture results.
Complications: NF has a high mortality and other complications include necrotizing myositis, septic shock and multiple organ failure.


Definition: Ecthyma gangrenosum is a cutaneous infection usually caused by Pseudomonas aeruginosa.
Aetiology: It is usually a manifestation of bacterial systemic infection with P. aeruginosa in immunosuppressed persons, including those with AIDS, diabetes mellitus and neutropenia.
Clinical presentation: Characteristically presents as tender pustules or haemorrhagic blisters with an erythematous edge that progress to form a central black eschar and ulcerate.
Epidemiology: Ecthyma gangrenosum is rare.
Diagnosis: Ecthyma gangrenosum is a clinical diagnosis and suspicion of the disease warrants a prompt tissue and blood cultures.
Prevention: Maintenance of personal hygiene and care of open wounds in immunosuppressed persons.
Treatment: On clinical suspicion, broad-spectrum empiric antibiotic therapy to include anti- pseudomonal coverage should be initiated. Options include aminoglycosides, fluoroquinolones e.g. ciprofloxacin or third-generation cephalosporins e.g. ceftazidime/ceftriazone. If the lesions fail to respond to antibiotics, surgical debridement may be required.



| Bacterial Infections | 1st line therapy | 1st line therapy | Alternative therapy |
|---|---|---|---|
| Impetigo | Topical therapy | Mupirocin | Fusidic acid |
| Systematic antibiotics | Flucloxacillin, IV cloxacillin | Macrolides e.g. Erythromycin | |
| Folliculitis | Topical therapy | Mupirocin | Macrolides |
| Systematic antibiotics | Flucloxacillin | Erythromycin, Cephalexin | |
| Furunculosis | As for folliculitis | ||
| Necrotising Fasciiitis | IV penicillin G, gentamycin and clindamycin | Fasciotomy as required | |
| Ecthyma gangrenosum | Ciprofloxacin, ceftazidime | ||
Definition: This refers to either invasion of the skin and mucous membranes with Mycobacterium tuberculosis or a hypersensitivity reaction to the organism.
Aetiology: M. tuberculosis can infect the skin and the route of infection and immune status of the person influences clinical presentation. Tuberculids and erythema induratum are hypersensitivity reactions usually seen in people with good immunity.
Epidemiology: Cutaneous TB is rare.
Diagnosis: Cutaneous TB is confirmed by a skin biopsy that shows characteristic features and a tissue culture.
Prevention: Vaccination, early detection, treatment and completion of the course are the mainstays of disease transmission in general. However, the risk of transmission in cutaneous TB is minimal.
Treatment: Six months standard intensive treatment with rifampicin, isoniazid, pyrazinamide and ethambutol for 2 months followed by the continuation phase with rifampicin and isoniazid is effective for cutaneous TB. However, in instances of severe or complicated disease it may be extended to nine months.
Complications: Miliary TB has a high mortality, scrofuloderma may be associated with severe scarring and contractures and lupus vulgaris may result in squamous cell carcinomas.