Acute bone infection in adults
by Pravesh Panchoo & Maritz Laubscher
Learning objectives
- Define acute osteomyelitis.
- Recognie a patient presenting with acute bone infection.
- Know the management of acute bone infections.
- Exclude immunocompromise and assess nutritional status.
Introduction
Bone infection also known as osteitis or osteomyelitis can be divided into acute, sub-acute and chronic osteomyelitis.
Acute osteomyelitis has an onset of 2 weeks or less. In subacute osteomyelitis, infection lasts from one to several months, after which chronicity begins. Chronic osteitis is characterised by progressive bone destruction and new bone apposition.
Pathophysiology
Haematogenous
Haematogenous spread in adults is rare. When it occurs, it usually affects the spine. Microorganisms seed to bone in the event of a bacteremia. The most common organism found in hematogenous spread is Staphylococcus aureus.
Contiguous spread
Infection spread from adjacent soft tissue to bone. It is mostly associated with non- healing wounds (diabetic foot, neuropathic ulcer, venous stasis ulcer).
Direct inoculation
Open fractures, penetrating injuries or bone surgeries can be a direct source of infection resulting in acute osteomyelitis.
Microbiology
Staphylococcus aureus is the most common organism involved.
Enterobacter, enterococcus, Pseudomonas and streptococcus species are sometimes isolated. Unusual organisms are sometimes isolated in specific population: Salmonella in patients with Sickle cell disease, fungal infection in immunosuppressed patients.
Clinical findings
History is important to categorize type of host and onset.
Symptoms
- Pain: Usually dull pain, even at rest and at night (RED FLAG). Can limit weight bearing.
- Fever: Varies from low to high grade fever, can be associated with chills and rigors in case of sepsis.
Physical examination
General examination: Should inform about the host status of the patient.
Local examination: Erythema, tenderness and oedema usually present. There can be an area of fluctuation, indicative of an associated soft tissue abscess. Presence of surgical scars should raise suspicion.
The patient refuses to weight bear if the lower limb is affected. The joints above and below must be assessed to exclude associated septic arthritis.

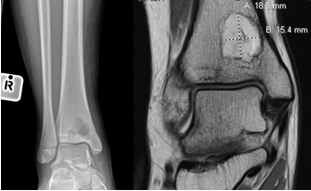
Radiographs
Anteroposterior and lateral views of the affected limb. May be normal in early infection. At a later stage periosteal reaction can be seen. Can also identify air around soft tissue suggestive of an infection. Involucrum and sequestrum are features of chronic osteomyelitis.

Brodie abscess
A Brodie abscess consists of a region of suppuration and necrosis encapsulated by granulation tissue within a rim of sclerotic bone. Brodie abscess occurs in the setting of subacute osteomyelitis in the metaphysis of long bones, typically in patients < 25 years of age. It is usually of hematogenous origin but can also occur in the setting of trauma.
The most common pathogen is S. aureus. The most common site is the distal tibia; other sites include the femur, fibula, radius, and ulna.
Computer tomography (CT) scan
CT is more sensitive than conventional radiography for assessing cortical and trabecular integrity, periosteal reaction, intraosseous gas, soft tissue gas, and the extent of sinus tracts. It is useful in chronic osteomyelitis and may be the most useful modality to evaluate for the presence of osseous sequestrum and involucrum.
Magnetic resonance imaging (MRI)
MRI is the imaging modality with greatest sensitivity for the diagnosis of osteomyelitis. After radiographic evaluation, MRI is generally considered the study of choice for further assessment. It is useful for obtaining images delineating the extent of cortical destruction characteristic of osteomyelitis, as well as to evaluate for presence of bone marrow abnormality, soft tissue inflammation (such as in the setting of cellulitis, myositis, and/or ulceration) and ischemia. MRI may demonstrate abnormal marrow edema as early as 1 to 5 days following onset of infection.
Laboratory investigations
- White cell count:raised white cell count with neutrophilia
- Erythrocyte Sedimentation Rate (ESR):normal range 0-10. Elevated in 90% cases. A decrease in ESR shows good response to treatment.
- C-Reactive Protein (CRP):normal range < 4. Most sensitive blood marker, elevated in 97% cases. Decreases faster than ESR.
- Blood cultures:their utility is mainly in hematogenous osteomyelitis where it is positive in about 50% cases.
- A workup for immunocompromise and malnutrition must be included if unknown (i.e.HIV, HBA1C, Albumin)
Microbiology
Tissue and bone samples sent during debridement help identifying the causative organism and guide antibiotic treatment.
Complications
- Sinus tract formation
- Contiguous soft tissue infection
- Abscess
- Septic arthritis
- Systemic infection
- Chronic osteomyelitis
Treatment
Non operative
Assessment for systemic signs of an infection is crucial and patients must be resuscitated in severe acute bone infections.
Antibiotic therapy alone without surgical debridement is an option in hematogenous osteomyelitis. It is then either guided by the result of blood culture or empirical, aiming at the most common organism (staphylococcus aureus). The duration of treatment is 4–6 weeks.
Operative
Surgical debridement for management of osteomyelitis consists of removal of necrotic material and culture of involved tissue and bone. A satisfactory soft tissue envelope overlying the site of infection must be re-established for successful treatment, either via direct closure or flap coverage. In the setting of non-viable or injured bone and/or infected fluid collections, surgical debridement is a cornerstone of therapy. Antimicrobial therapy alone is not effective for cure of infected, necrotic bone
Key takeaways
- Acute bone infections in adults mostly caused by direct inoculation or contiguity
- Staphylococcus aureus is the most common organism involved
- Radiographs can be normal at the beginning, so high index of suspicion needed.
- MRI is presently considered the most sensitive examination for detection of early infection
References
- Mark D. Miller, Stephen R. Thompson: MILLER’S REVIEW OF
- ORTHOPAEDICS seventh edition
- Louis Solomon, David Warwick, Selvadurai Nayagam: APLEY’S SYSTEM OF ORTHOPAEDICS AND FRACTURES
- Charles E Spritzer: Approach to imaging modalities in the setting of suspected nonvertebral osteomyelitis.
- Tahaniyat Lalani, Steven K Schmitt:Osteomyelitis in adults: Clinical manifestations and diagnosis
- Douglas R Osmon,Aaron J Tande: Osteomyelitis in adults: Treatment